Recurrent UTI Treatment: Which Approach Is Right For You?
Jump To Section:
- Short course antibiotics for UTI treatment. >>>>
- Prophylactic antibiotics for recurrent UTI. >>>>
- Long term antibiotics for UTI. >>>>
- Estrogen for recurrent UTI treatment. >>>>
- Other UTI remedies and treatment options. >>>>
- Recurrent UTI treatment specialists. >>>>
The truth is, there are very few conclusive guidelines for recurrent UTI treatment. If you show up at a clinic with yet another UTI, you will most likely receive a short course of antibiotics – the same treatment you would receive if it was your first UTI.
 | “My doctor just gives me a prescription for Nitrofurantoin each time. I’ve been using the same antibiotic for years. She used to test my urine with one of those strips, but now she trusts that I know I have a UTI. Sometimes she just calls in my script so I don’t need an appointment.” |
This would be all well and good if it cleared up your recurrent UTIs and you didn’t end up back at the doctor or pharmacy for yet another course of antibiotics every few months.
If you take antibiotics each time you get a UTI, but you continue to get UTIs, you should question whether the antibiotic is working at all.
What Happens When A UTI Is Not Properly Treated?
We all know a little something about bacteria. We commonly group bacteria with other pathogens, like viruses, into one big group called germs. And we’re all aware of the role germs play in illness and infections.
You may not know that bacteria can be found as free-floating cells, or clustered together in communities called biofilms. In an uncomplicated urinary tract infection, free-floating bacteria can be detected in the urine with appropriate testing, then treated with the right antibiotic.
Without fast and effective treatment, bacteria in the bladder may attach to the bladder wall and begin to form a biofilm community. Once attached, the bacterial community generates a slimy protective coating that creates a safe environment and shields it from outside influences.
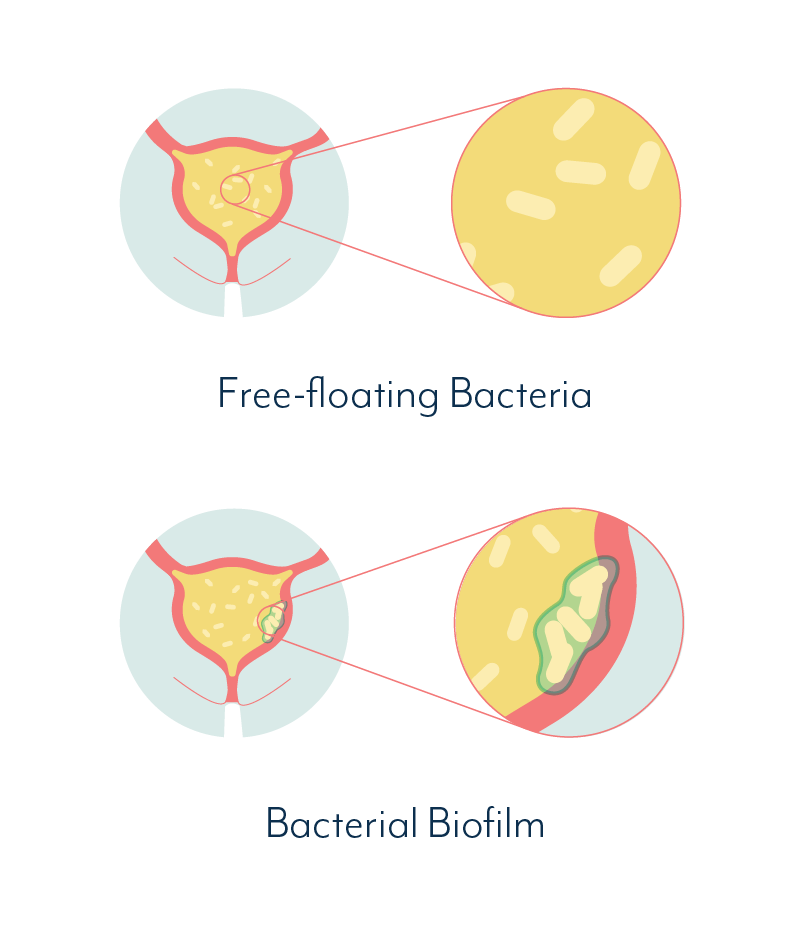
When a biofilm reaches this stage, it is extremely resistant to antibiotics, as well as the body’s natural defence mechanisms. This is where a chronic infection begins. You might refer to it as recurrent UTI or chronic cystitis – the kind of urinary tract infection that just keeps coming back.
Check out our expert video series to learn more about how biofilm contributes to antibiotic resistance in chronic UTI.
 | “I would have episodes of excruciating pain, blood in my urine and that smell that just tells you that you have a UTI. Then sometimes I would feel practically normal. All the other days in between, I had these niggling symptoms, constantly threatening to blow up at any given moment.” |
Can UTI Treatment Succeed If Biofilms Are Involved?
Biofilms that cause chronic urinary tract infections can be difficult to detect and very hard to treat efficiently. Currently, no guidelines exist to help clinicians and microbiologists detect and treat biofilm infections of the urinary bladder.
 | “Most UTI guidelines are aimed at management of simple uncomplicated UTI. It can be very difficult to successfully manage complex or recurrent UTI in primary care. If symptoms persist, or where there is diagnostic uncertainty GP’s will need to make a referral for specialist assessment." |
Free-floating bacteria behave very differently to bacteria within a biofilm. Bacteria growing as biofilms are also much more difficult to identify in a urine sample.
No three or five day course of antibiotics designed to treat free-floating bacteria is even going to make a dent on your average biofilm.
As much as we do know about biofilms, the mechanisms behind this phenomenon are still poorly understood. To add another layer of doom, biofilms can be formed by one or multiple species, in complex structures.
If the right treatment is found for one of the species in a biofilm, as its prominence decreases, a second species may rise to take its place.
This doesn’t necessarily mean treatment is impossible, but it can take a few rounds of different targeted antibiotics to get to the bottom of a multiple-bacteria biofilm. Learn more in our dedicated section on chronic UTI and biofilm.
As far as recurrent UTI treatment options, it pays to understand the pros and cons. There are a few to delve into:
- Short course antibiotics
- Prophylactic antibiotics
- Long term antibiotics
- Estrogen therapy
- Other non-antibiotic UTI therapies
Let’s take a look at each in more detail.
Short Course Antibiotics For UTI Treatment
When prescribed an antibiotic for uncomplicated UTI treatment, the course duration will usually be 3, 5 or 7 days (or longer if a kidney infection is suspected), depending on the antibiotic prescribed. Single dose antibiotics, such as Fosfomycin (Monurol), are also prescribed in some cases.
Common short course antibiotics are listed in our UTI antibiotics section, with their potential side effects. And antibiotic treatment for UTI in men is described in our article on male UTI treatment. We won’t go into detail here for the following reason…
Short courses of antibiotics are not designed for recurrent UTI treatment. Particularly not those recurrent UTIs that are caused by an underlying bladder infection that has been around for months or even years.
What Is The Best Antibiotic For UTI?
We see hundreds of questions in forums, along the lines of, “Can I use (insert random antibiotic here) for a UTI?”
It is important to understand that there is no such thing as “the best antibiotic for a UTI.”
There IS such a thing as the best antibiotic for the specific type of bacterium (or multiple bacteria) causing YOUR UTI. Antibiotic susceptibility testing can help identify possible treatment options.
And although some types of bacteria are more common than others when it comes to causing UTIs, it’s really important you realize, the cause of YOUR UTI is unlikely to be the same as the cause of a random online stranger’s UTI.
Just because their UTI treatment was successful, it does not mean the same UTI treatment will work for you.
More importantly, there is increasing doubt over whether short course antibiotics provide any benefit at all in cases of recurrent UTI caused by a persistent, embedded bladder infection.

“I always took antibiotics as soon as I felt UTI symptoms. It would pretty much clear up by the next day. Then I got a UTI when I didn’t have my antibiotics with me. I freaked out, but by the next day it had cleared up anyway. Now I have no idea whether the antibiotics even help.”
Temporary flare ups of UTI symptoms caused by a chronic infection may or may not be relieved faster than when non-antibiotic treatments are used. This means, the antibiotics you rely on for UTI treatment every time you get symptoms may not be making any difference whatsoever.
And if the infection is not cleared, a recurrence is almost certain.
Ineffective antibiotic treatment may also contribute to bacterial resistance, making the UTI even harder to treat.
Prophylactic Antibiotics For Recurrent UTI Treatment
Prophylactic antibiotics for recurrent UTI treatment sounds complicated, but in reality, it just means preventative antibiotic use. That is, you use antibiotics before you feel any UTI symptoms, in the hope of preventing one from happening at all.
We want to state straight up that there is evidence that long-term prophylactic antibiotics for recurrent UTI treatment do not alter the long-term risk of recurrence.
This basically means that patients with recurrent UTIs who take prophylactic antibiotics may experience a decrease in frequency of symptoms during prophylaxis (that is, while they are taking the antibiotics).
But when they stop prophylaxis, their acute episodes return at the same rate as before their UTI treatment started. This was Emma’s experience with prophylactic antibiotics.
Ultimately, long-term prophylactic antibiotics do not appear to alter a patient’s basic susceptibility to infection in most cases.
How Prophylactic Antibiotics Are Taken
There are two main approaches to prophylactic antibiotics for recurrent UTI treatment:
- Postcoital prophylaxis – in sexually active females, a single dose of antibiotic post-sex
- Continuous prophylaxis – a long-term low dose of antibiotic, usually a single dose daily
Postcoital prophylaxis appears to have similar effectiveness but fewer side effects than continuous prophylaxis for preventing recurrent UTI. This is mainly because females on postcoital prophylaxis generally take fewer doses of the antibiotic.
A third type of UTI treatment often grouped with prophylactic options is acute self-treatment. This is a “self-start” approach where a patient is provided prescriptions for antibiotics, and can initiate their own standard 3-day course when they feel UTI symptoms coming on.
Acute self-treatment is recommended for ≤2 episodes of UTIs per year or for females who are not suitable candidates for longer term prophylaxis. Continuous or postcoital antibiotic prophylaxis are generally considered suitable for ≥3 episodes of UTIs each year.
Interestingly, studies into prophylactic antibiotics for recurrent UTI treatment have demonstrated that patients are highly accurate in diagnosing their own UTIs. So keep this in mind the next time you receive negative UTI test results – if you think you have a UTI, it’s quite likely you do. The test is probably wrong, not your intuition.
 | “I had had so many UTIs over the course of 2 years, my doctor decided it was a fairly safe option to prescribe postcoital antibiotics. I took them for a few months, but then I stopped, and the UTIs just came back.” |
The Pros And Cons Of Prophylactic Antibiotics For UTI Treatment
| PROS | • Studies show, that for the duration of prophylactic antibiotics for UTI treatment, females experience up to a 95% reduction in UTI recurrences. • Our interviewees that rely on prophylactic antibiotics find the anxiety related to a potential recurrence is reduced with the knowledge that it is less likely. |
| CONS | • Studies show that once prophylactic treatment is ended, females are likely to return to the same rate of UTI recurrence they experienced before they commenced the treatment. • Any type of antibiotic use comes with potential side effects, which include destroying good bacteria in the gut and increasing the risk of yeast infection. • Research has found that prophylactic antibiotics for UTI treatment promote the development of antibiotic-resistant forms of UTI-causing E.coli (uropathogenic E.coli, or UPEC). |
This last point is extremely important. Without even knowing it, by taking ineffective antibiotics you could be encouraging a difficult-to-treat embedded infection to form in your urinary tract.
For this reason alone, specialists in the area of chronic urinary tract infections do not recommend the use of low dose antibiotic regimens for UTI treatment.
So while you may find prophylactic antibiotic treatment helpful, there is a good chance your UTIs will return if you cease the treatment, and you may actually be making your condition worse.
Long Term Antibiotics For UTI
Treatment of biofilms or embedded infection within the bladder may take a longer term approach.
We’ve discussed elsewhere on our site the difficulty of treating an infection encased in a biofilm, or within the bladder wall.
Bacteria can live for 6 months or more protected within their biofilm or within the bladder wall. The long-term duration of treatment is in part considered necessary because of this lifecycle.
Periodically, bacteria may escape from a biofilm and either be flushed from the body, or attach to the bladder wall to form new biofilm communities.
The idea behind a constant regimen of high dose antibiotics over six months or more, is that any bacteria that do escape into the urine will hopefully be eradicated before reattaching to the bladder wall.
And eventually, the lifecycle of the already embedded bacteria will also have come to an end.
The best case scenario with long term high dose treatment is that the bacterial community within any biofilm is destroyed.
The main difference between this type of UTI treatment, and the continuous prophylactic antibiotic treatment mentioned above, is the dosage.
Prophylactic doses are low, and are intended to prevent acute episodes. Biofilm treatment doses are high, and are intended to eradicate the infection completely over time.

“For the cases I see, on average it takes a year of antibiotic treatment to resolve their symptoms, but there’s a wide variance. There are some people with infections we can’t get rid of, and we have to control the symptoms.”
This type of treatment shouldn’t be attempted alone. It’s essential to work with a clinician that can oversee treatment and assess the use of antibiotics. As we all know, antibiotics can come with side effects, and these can be serious.
One protocol for long term antibiotic treatment for chronic UTI has been demonstrated in the UK, and an alternative approach to oral antibiotics is antibiotic bladder instills, which some people may respond to better.
Check out our interview with Dr. David Kaufman where we discuss his approach to long term antibiotics.
Estrogen For Recurrent UTI Treatment
Can estrogen help for recurrent UTI?
We’ve covered this in detail in our content on UTI and Menopause, but for a quick overview…
Post-menopausal females that experience recurrent UTI may be prescribed hormone replacement therapy (HRT). This could be estrogen in a systemic form (a pill taken orally) or topical form (a cream that is applied inside the vagina).
So why estrogen? And why in the vagina?
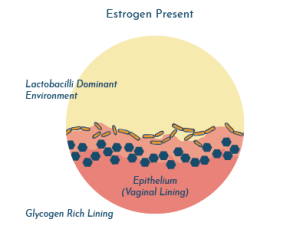
Science has shown that the vaginal and urinary microbiomes are interconnected, and it would appear that a healthy vaginal environment with a good amount of lactic acid can provide some protection from UTIs.
To maintain this healthy vaginal environment, it’s important that Lactobacilli are abundant. These Lactobacilli multiply when the right source of food is readily available. In this case, that source of food is glycogen that is found on the surface of the vaginal epithelial cells (vaginal lining).
The more glycogen that is available, the more the Lactobacilli eat, and the more they multiply. It is thought that estrogen increases the stores of glycogen.
When females go through menopause, the levels of estrogen are reduced, resulting in diminished glycogen stores, and therefore the Lactobacillus population is also reduced.
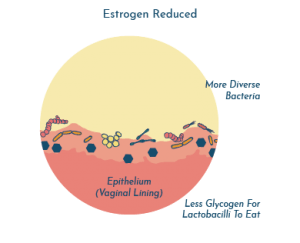
Studies have shown that estrogen therapy may help reverse this process and result in a reduced risk of UTI.
Learn more about estrogen treatment for UTI.
Other UTI Remedies And Treatment Options
While there are many studies aimed at measuring the effectiveness of different antibiotics for UTI treatment, there is very little solid research around non-antibiotic treatment of UTIs. We’ve covered the most searched for UTI home remedies in detail in a separate article.
A number of researchers have questioned whether antibiotics should be the go-to for first-time uncomplicated urinary tract infections, suggesting they may be unnecessary in many cases.
Because diagnosis and treatment guidelines are based on evidence, and because natural remedies are rarely studied, they are not found within therapeutic guidelines, and your doctor is very unlikely to recommend them.
So what are the non-antibiotic treatment options for recurrent UTI?
Bacteriophage Therapy For Recurrent UTI
Bacteriophage therapy, or phage therapy, can sound somewhat sci-fi, but in reality, it is based on a process that is continuously occurring in our bodies. Phages are just one of the organisms that helps keep a healthy microbiome in check.
Phages are viruses that infect and destroy specific bacteria. They are naturally programmed to seek out and kill a particular type of bacterium, such as E. coli, and they will not impact anything else in the microbiome.
For this reason, phage therapy has gained popularity as a potential therapy for antibiotic resistance and difficult-to-treat infection. In reality, phage therapy is not new, but research was abandoned in many parts of the world with the discovery of antibiotics.
Is phage therapy an option for sufferers of recurrent or chronic UTI? Maybe. We’ve covered phage therapy for UTI in detail, so you can learn all about it.
Fulguration For Recurrent UTI
Although bladder fulguration has become a popular topic in recent years, the procedure itself has been around for decades. The process includes inserting a tool through the urethra, similar to that of a cystoscope, and cauterizing abnormal lesions on the bladder wall.
The purpose of bladder fulguration for recurrent UTI is to remove lesions which may be harboring bacteria of which antimicrobials are unable to reach. While some patients have reported great success, others experience no change or a worsening of symptoms.
As far as the scientific research goes, for the most common type of tissue change, trigonitis, up to 90% of patients report symptom improvement or fewer UTIs per year. But for the more rare tissue abnormalities, such as leukoplakia, vesicular cystitis, and Hunner’s ulcers, the rate of success is closer to 50%, with some requiring repeat fulguration.
We brought all of the information from clinicians, patients, and research together to discuss fulguration for recurrent UTI.
Should You Try UTI Home Remedies?
The only person that can make this decision is you. And before deciding, you should learn what you can about any UTI remedy you’re considering.
And it’s important to understand this:
The absence of evidence around non-antibiotic UTI treatments does not mean they do not work, but it does mean we don’t know if they work.
Just because a number of people agree in a UTI forum that a particular remedy works for them, it does not mean it will work for you, or that it even works at all.

Think about it… If you rely on a specific home remedy every time symptoms of a UTI flare up, yet you continue to get UTIs, you can almost guarantee that remedy is not addressing the underlying problem.
Obviously, this does little to curb the enthusiasm for natural UTI remedies online. There is always plenty of discussion on how to treat your next UTI, but very little around resolving the issue so it never happens again.
It’s essential to separate the myths from fact – there are natural UTI remedies that are looking very promising as future UTI treatment options, but there are other very well publicized natural UTI remedies that have been proven ineffective.
It can be difficult to figure out who to believe. So in our UTI home remedies article we’ve taken a look at how home remedies stack up, including D-mannose and vitamin C.
Recurrent UTI Treatment Specialists
Finding the proper specialist to treat your UTIs is an important step, as discussed by UK reality TV star Marnie Simpson who has also dealt with a chronic UTI. There are very few practitioners who specialize in the treatment of recurrent urinary tract infections, but we maintain a list by region of those we have come across in our research.
Watch our video interview with Dr. Mandy, who discusses the importance of the immune system when trying to tackle recurrent UTI.
If you would like more information on specialists in your area, it’s best to get in touch with us directly and let us know where you’re based. We can’t guarantee we can help, but we’re always working on expanding our network.
And please get in touch if you would like to recommend a practitioner who has helped you!
If you’d like to learn more about some of the different primary care and urology approaches, check out the article and video links below:
- Dr. Michael Hsieh (USA)
- Dr. Cat Anderson (UK)
- Ruth Kriz (USA, retired)
- Dr. Philippe Zimmern (USA) (read Carrie’s story about working with Dr. Zimmern)
- Dr. Stewart Bundrick (USA)
- Dr. Timothy Hlavinka (USA)
- The late Professor Malone-Lee (UK)
- Dr. Raj Patel (USA)
- Dr. Angelish Kumar (USA)
We’ve also covered naturopathy, neuralgia, health psychology and pelvic floor physical therapy:
- Dr. Nicholas Fogelson, Neuropelveology (USA)
- Dr. Ashley Girard, Naturopathic Doctor (Canada)
- Aline Filipe, Pelvic Floor Physiotherapist (Australia)
- Dr. Bri, Pelvic Floor Physiotherapist (Online only)
- Dr. Sula Windgassen, Health Psychologist (UK)
Clinicians who would like to get involved in our community can learn more on our clinician information page.
The Steps To Overcoming Recurrent UTI
For those of us who experience persistent UTI, the treatment options can seem pretty grim.
We’ve covered short course antibiotics, which are unlikely to resolve recurrent UTIs caused by a chronic bladder infection and may not even help with symptoms.
Then there’s prophylactic antibiotics for UTI treatment, which can reduce episodes of recurrence while you’re on it, but once you stop, you could be right back where you started, or in an even worse position.
Not to mention the havoc frequent or long-term antibiotics can wreak throughout your body.
So what are the options here? We’d love to say we can point you in the right direction for a guaranteed cure, but, as we’re sure you’ve guessed, it’s not that simple.
UTI Treatment: Steps To Success
There are multiple parts to this problem. First, learn everything you can about recurrent and chronic UTI.
Then, the success of your journey will depend on four things:
- Collecting a high quality urine sample
- Pursuing more accurate UTI testing
- Working with a specialist that understands recurrent UTI and can help with 1 and 2
- Having the perseverance to find another doctor if step 3 doesn’t work out
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions and comments below, or get in touch with our team.


Hello, please send a list of providers in Michigan. Thank you.
Hi TP, I’ve sent this via email. Best wishes,Issy
I have reoccurring utis every month and Its ruining my life. D mannose works sometimes but I am so scared. I tried prophppactic antibiotics a year ago it didn’t work. My urologist gave up, im so scared please I need help the finding a doctor. I’m in OR in the US and I have BCBS/Anthem insurance. Willing to travel
Hi Hannah,
I’ve sent an email with this information
Best wishes,
Issy
Hello, I’m based in Chicago and would appreciate any recommendations for specialists in the area and in the US – I’m willing to travel. Thank you.
Hi there, I’ve sent an email with this information to you. Best wishes, Issy
Hello! Hoping you have a list of recommended providers in OR? The only one I can find doesn’t accept my insurance (CIGNA), and I’m really hoping to remedy my chronic UTIs. Thanks!
Hi Courtney, I’ve sent you an email with this information. Best wishes, Issy
Do you have contacts for Chronic UTI specialists in Oregon? (or WA or CA)
Hi Julie, I’ve sent you a list of practitioners for these states. I hope this helps, Issy
Do you have details for a UTI specialist in South London? Or in the London area.
Author
Hi Imogen, we sent further information by email – I hope it’s helpful. Melissa
Hi I have lost your email, please can you resend?
Hi Imogen, I’ve sent you an email. Best wishes, Issy
Hi! I’ve had UTI like symptoms for the last year. I’ve taken multiple test and all negative. I’ve tested for STDs and negative. Some days the symptoms are very mild to nonexistent and some days particularly in the mornings it’s a dull ache in pelvic area and slight burning when I pee. No excruciating pain. There was no blood in urine and urologist performed coposcopy and bladder was healthy and no cancer present. I am at a loss why this won’t go away.
Author
Hi Davita, it can be helpful to consult with a recurrent/chronic UTI specialist for an additional opinion. If you send us a direct message and let us know where you are based, we can share more information. It’s also possible that another condition could be causing urinary symptoms, so it can be beneficial to keep investigating. Melissa
Hi. I’m based in the UK, Newcastle. Does anyone know any UTI specialist here please??
Author
Hi Naghmeh, we sent you an email with more information a few days ago. I hope it’s helpful, Melissa
Hi, do we know any specialists in Sweden? Thank you so much!
Author
Hi Mag, we sent you an email and you’re welcome to ask any further questions there. Melissa
Looking for a specialist in Denver, CO. Get about 5 UTIs per year- recent urogynecologist wrote me off when recent test came back negative despite symptoms. A few years ago I had 16 confirmed utis in one year. Need someone who can help me.
Author
Hi Samantha, we sent you an email with more information. I hope it’s helpful, Melissa