UTI Antibiotics: Treatment For Urinary Tract Infection
What are the best UTI antibiotics? What happens if antibiotics don’t work? Can you treat a UTI without antibiotics?
Here is where we lay out everything you need to know about UTI antibiotics. If you’ve ever googled questions like…
Should I take Amoxicillin for UTI?
What are the best antibiotics for UTI?
Is Macrobid for UTI appropriate?
What happens if antibiotics don’t work for UTI?
Can you treat a UTI without antibiotics?
This article is for you. Even if you haven’t googled any of these, but have questions about antibiotics for UTI, this should have you covered.
Jump To Section:
- How UTI antibiotics are selected. >>>>
- What happens if antibiotics don’t work for UTI? >>>>
- My UTI test results are negative, what now? >>>>
- Do I have recurrent UTI or Interstitial Cystitis? >>>>
- Can you break the UTI antibiotic treatment cycle? >>>>
We find people discuss UTI antibiotics as though this represents a single treatment option. In reality, UTI antibiotics refers to a whole range of different drugs and doses, selected for specific reasons.
Knowing why certain antibiotics are helpful and others aren’t will give you more control over your own treatment. So let’s start at the very beginning. That way you can confirm the knowledge you already have, then expand on it.
UTI Treatment Antibiotics Overview
When faced with an uncomplicated urinary tract infection, your three main treatment options are antibiotics, natural remedies, or riding it out with nothing but water.
Can you take just any antibiotic for bladder infection?
The short and very decisive answer to that is no.
Every antibiotic is processed by our bodies differently. Some antibiotics, when taken orally, will never pass through the urinary tract. Or if they do, it is in such small amounts as to be completely ineffective.
Self-prescribing antibiotics could result in you taking medication that has zero positive impact, and possibly negative side effects.
Even if google tells you that whatever you have on hand does indeed pass through the urinary tract, do you know what types of bacteria it treats? More importantly, do you know which bacteria (or other pathogens) are causing your symptoms?
Most people don’t have the answers to either of these questions when they opt to self-treat a UTI. Below we’ve provided crucial information for you to consider.
How UTI Antibiotics Are Selected
Clinical and therapeutic guidelines for urinary tract infections guide medical practitioners on how to make a diagnosis. On top of this, the guidelines may help them select an appropriate treatment.
However, when it comes to choosing an antibiotic to treat any infection, there is a whole long list of things that can influence a doctor’s decision:
 | “No single [antibiotic] is considered best for treating acute uncomplicated cystitis... Choosing an antibiotic depends on [its] effectiveness, risks of adverse effects, resistance rates, and… Additionally, physicians should consider cost, availability, and specific patient factors, such as allergy history.” |
Without accurate test results, none of these things mean much, and the choice of any antibiotic is really just an educated guess.
UTI Antibiotics Effectiveness
Currently, there is no testing method that allows a medical practitioner to find out what is causing the infection when you show up at a clinic with a UTI. They rely on their experience, your awareness of your own body and symptoms, and at times, a strip test.
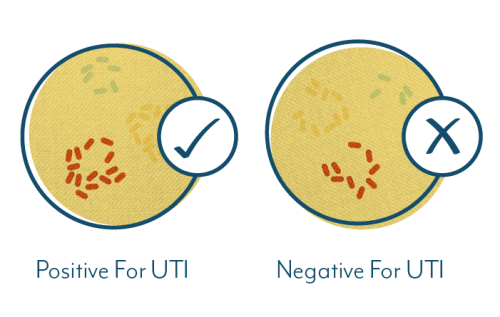
If you’ve read through our UTI testing section, you’ll know this strip test is not designed to reveal what is causing your infection. It is only a tool to help identify whether there is an infection present. And it is a highly inaccurate tool.
So let’s recap. Your doctor can fairly accurately deduce whether you have a UTI, but at the time you show up at the clinic, three things remain unknown:
- Which bacterium or other pathogen is causing your infection (and there may be multiple)
- Which classes of antibiotic are appropriate for use on that bacterium
- How resistant that bacterium is to the different antibiotic classes
If your urine is tested, and the test is accurate (see our section on testing inaccuracy), all three of these can be answered. But this takes 2-3 days (see below for what happens then).
First Line UTI Antibiotics: A Best Guess Treatment
If you are prescribed a UTI treatment antibiotic when you show up at a clinic, it can only be selected according to the following criteria:
- What type of bacteria is most likely to have caused an uncomplicated UTI, given the region you are based in
- Which antibiotic the guidelines recommend for treating that most common type of bacteria
In the US, we have a rough idea of the most common causes of UTIs. E.coli is currently considered the most likely cause, and antibiotic resistance patterns are monitored in each region. This means doctors have access to information that allows them to narrow down which antibiotic is likely to be effective for a UTI caused by E.coli in their particular region.
If your doctor requests a urine sample for lab testing, it is probable they will also prescribe the first line antibiotic for your region. In doing this, they are hedging their bets while they wait for your test results.
You can explore our expert video series to learn more about treatment approaches when multiple bacteria are present.
 | A first line antibiotic for a urinary tract infection is the antibiotic that is generally accepted by the medical authority of the region as being the most likely to result in successful treatment. |
Can I Change UTI Antibiotics?
The probability that the first line antibiotic will be effective is relatively high. But what happens if UTI antibiotics don’t work?
This is where that sample that was sent off for testing should help.
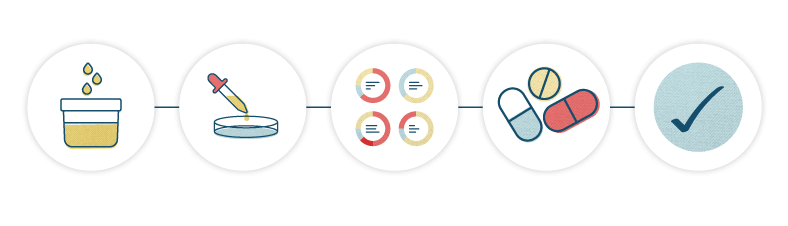
In the event your symptoms are not reduced, the lab test should identify which antibiotic will work better. In order to identify which antibiotic is likely to be effective, antibiotic susceptibility testing is conducted.
What is antibiotic susceptibility?
Simply put, antibiotic susceptibility is a measure of how sensitive a particular type of bacterium is to a particular antibiotic, or to a range of different antibiotics.
Antibiotic susceptibility testing is the practical application of this. In the lab, different antibiotics are physically applied to the bacteria found in your sample. This is then observed, and it is noted whether the antibiotic inhibits the growth of the bacteria, and if so, by how much.
The results of an antibiotic susceptibility test can help your doctor choose which antibiotic to recommend, particularly when the first round of treatment failed.
Although antibiotic susceptibility testing is helpful in theory, if you’ve read our section on testing, you’ll know that this process is not foolproof. And if an infection has become chronic or embedded, even a short course of the right antibiotic will not address the underlying infection.
Adverse Effects Of UTI Antibiotics And Specific Patient Factors
If you’ve ever read the leaflet that comes with your UTI antibiotics, you will know there are many side effects that can occur with antibiotic use. Certain people react to certain antibiotics, and some antibiotics are much more likely to cause side effects than others.
Side Effects Of Common Antibiotics Used To Treat Uncomplicated UTI
| Antimicrobial Agent (Brand) | Duration Of Course | |
|---|---|---|
| Trimethoprim–sulfamethoxazole (Bactrim, Septra) | 3 days | |
| Possible Side Effects: | ||
| Fever, rash, photosensitivity, neutropenia, thrombocytopenia, anorexia, nausea and vomiting, pruritus, headache, urticaria, Stevens–Johnson syndrome, and toxic epidermal necrosis | ||
| Trimethoprim (Trimpex, Primsol) | 3 days | |
| Possible Side Effects: | ||
| Rash, pruritus, photosensitivity, exfoliative dermatitis, Stevens–Johnson syndrome, toxic epidermal necrosis, and aseptic meningitis | ||
| Nitrofurantoin monohydrate/macrocrystals (Macrobid) | 7 days | |
| Possible Side Effects: | ||
| Anorexia, nausea, vomiting, hypersensitivity, peripheral neuropathy, hepatitis, hemolytic anemia, and pulmonary reactions | ||
| Fosfomycin tromethamine (Monurol) | Single dose | |
| Possible Side Effects: | ||
| Diarrhea, nausea, vomiting, rash, and hypersensitivity | ||
| Amoxicillin and Clavulanate potassium (Augmentin, Augmentin ES-600, Augmentin XR) | Varies | |
| Possible Side Effects: | ||
| Hives or welts, itching, itching of the vagina or genital area, pain during sexual intercourse, redness or rash of the skin, thick, white vaginal discharge with no odor or with a mild odor, bloody or cloudy urine, fever, greatly decreased frequency of urination or amount of urine, seizures, swelling of the feet or lower legs | ||
| Ciprofloxacin (Cipro) Levofloxacin (Levaquin) Norfloxacin (Noroxin) Gatifloxacin (Tequin) | 3 days | |
| Possible Side Effects: | ||
| This class of antibiotics is known as fluoroquinolones and has been linked to serious side effects: Nausea, diarrhea, headache, dizziness, lightheadedness, trouble sleeping, rash, confusion, seizures, restlessness, Achilles tendon rupture, severe hypersensitivity, numbness in the arms or legs, confusion, hallucinations, hypoglycemia that can lead to coma, and hyperglycemia. |
||
Source: Treatment of Urinary Tract Infections in Nonpregnant Women
Are Fluoroquinolones Safe For Urinary Tract Infection?
The FDA has released numerous warnings advising against the use of fluoroquinolones.
 | “Fluoroquinolones should not be prescribed for patients who have other treatment options for... uncomplicated urinary tract infections (UTI) because the risks outweigh the benefits in these patients and other antibiotics to treat these conditions are available.” |
FDA-approved fluoroquinolones include levofloxacin (Levaquin), ciprofloxacin (Cipro), ciprofloxacin extended-release tablets, norfloxacin (Noroxin), moxifloxacin (Avelox), ofloxacin and gemifloxacin (Factive) – three of which are on the list of common antibiotics above.
As you can see above, side effects from antibiotics can get quite serious, so this is an important consideration.
Although one class of antibiotic may be considered the most effective for a particular type of bacteria, it may also come with an increased chance of severe side effects. This may mean for example, that Cipro for UTI is not your best option if there are other, non-fluoroquinolone antibiotics to choose from.
In this case, your doctor may opt for an antibiotic that has a reduced chance of success but is much safer.
UTI Antibiotics Resistance Rates
The breakdown of causes of urinary tract infections is not the same the world over.
While the same major groups of bacteria are generally identified everywhere, the percentage of infections caused by each, and the resistance of each to particular antibiotics is often different, depending on the region.
To put it simply, an antibiotic that is considered effective in one region may be considered less effective in another.
For this reason, each region has its own recommendations for first line antibiotics for urinary tract infections.
As we covered above, doctors use these recommendations to select which antibiotic to prescribe in the absence of conclusive test results. Recommendations change over time as bacterial resistance and prevalence changes. So medical practitioners need to keep up with the latest information.
It’s a tough job keeping up, and in reality, it is thought that up to 50% of antibiotic prescriptions in the United States continue to be unnecessary or inappropriate. This figure applies not only to UTI antibiotics, but to all prescriptions for antibiotics.
Check out our expert video series to learn more about antibiotic resistance in chronic UTI.
UTI Antibiotics Cost And Availability
Although one antibiotic may be considered more effective than another, it isn’t always realistic for your doctor to prescribe it. The preferred antibiotic may not be available in your region, or a high cost may outweigh the potential benefit.
Your doctor has to weigh up all these factors and make a decision on how to treat your UTI.
Without test results that clearly specify which type of pathogen is causing your infection, and how susceptible that particular pathogen is to different types of treatment, the decision is based on probability, reason and educated guesses.
This brings us, once again, back to the issue of ineffective antibiotic treatment and its possible contribution to the recurrence of urinary tract infections.
Ineffective antibiotic treatment may allow bacteria to increase their resistance to that type of antibiotic. As the antibiotic resistance of a bacterium grows, it becomes harder to treat. At this point it is even more important to test for its susceptibility to future treatment options.
Given that test results take 2-3 days, your doctor must either prescribe an antibiotic without knowing what is causing your UTI, or advise you to wait until the test results come back.
When prescribing UTI antibiotics, it is crucial for a doctor to select the right antibiotic, at the right dose, for the right amount of time. For all this to be possible, they must also make the correct diagnosis. And to do that, accurate testing is essential.
Why Aren’t My UTI Antibiotics Working?
What happens if your antibiotics don’t work for UTI?
There are a number of reasons your UTI antibiotics may not be working to eradicate your UTIs for good:
- You may not be taking the right antibiotic to treat the specific cause of your UTI
- Your symptoms may be caused by more than one organism, and antibiotic susceptibility testing for the entire bacterial community may be more relevant
- The duration of your treatment may be insufficient
- Your UTI symptoms may not be caused by bacteria
- An embedded, antibiotic-resistant infection involving a biofilm may be present in your bladder, requiring specialized, longer term treatment (read one example of this approach from our interview with Ruth Kriz)
In all of these scenarios, the only way to find an answer is to get accurate testing to identify the cause of your symptoms. Unfortunately, standard testing can be very inaccurate, and you may find yourself with negative test results despite your acute symptoms.
The Problems With Frequent Antibiotic Use
Our own research has shown that many females with recurrent UTIs have taken the same antibiotic for years. For some this can mean every few weeks; for others every few months.
 | “My doctor just calls in a prescription for the same antibiotic to whichever pharmacy I need them at, then I collect them. When I’m overseas I stock up on cheap antibiotics if I can get them. I’ve been taking the same antibiotic at least 15 years.” |
The longer you suffer from recurrent UTIs, the muddier the waters of UTI treatment antibiotics can seem. After all, if the treatment options you’ve tried have failed to prevent further UTIs, are any of them really working?
For many people, taking UTI antibiotics frequently is concerning. Yet without having found an effective alternative, antibiotics are still their first port of call at the onset of a UTI.
On a basic level, frequent antibiotic use means organizing multiple prescriptions, planning ahead and spending money. But there is also serious concern around antibiotic-resistant superbugs, destroying your gut flora, and whether frequent antibiotic use even helps.
And as we mentioned in our section on what causes UTIs, there is enough evidence to suggest that ineffective antibiotic use could be a major contributor to the formation of chronic infection, embedded in the bladder wall.
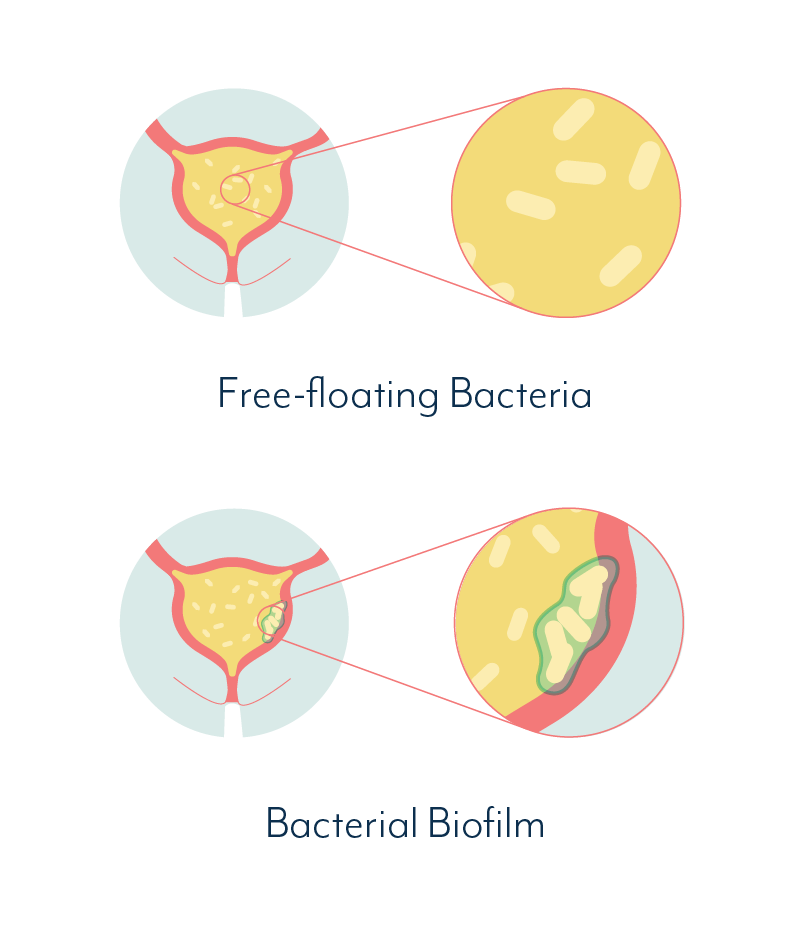
These types of infections typically involve biofilms – communities of bacteria that are very difficult to treat. The presence of biofilms can cause your symptoms to come and go, making you feel as though you get better, only to get another UTI…
Frequent antibiotic use that does not effectively treat chronic infection, can result in increased bacterial resistance, which again makes treatment more difficult.
Despite this, some of our community members have told us they reach a point where none of this matters enough to make them seriously reconsider their treatment. They are in pain, and they believe UTI antibiotics help ease it quickly.
Recurrent UTIs interfere with their daily lives and they rely on their antibiotics to help them get back to normal quickly.
No other solution has been offered to them, so UTI antibiotics become the only trusted weapon in a sea of remedies.
If this sounds familiar, it’s time to make sure you understand exactly what you’re taking and why. Hopefully we can teach you something you don’t already know.
My UTI Test Results Are Negative, What Now?
In an ideal situation, urinary tract infections would be easy to diagnose…
Your urine would be tested, the test would show what pathogen is causing the infection, and susceptibility testing would indicate the perfect antibiotic or other treatment for that pathogen.
Your doctor would prescribe the right treatment, your UTI would clear up, and you’d never have to think about it again. No more recurrent UTIs.
If you’re reading this site, we’re guessing there’s a good chance you have personal experience that is quite contrary to that ideal scenario.

“I could actually see blood in my urine and it was excruciating to pee. The doctor said it was obvious I had a UTI. I couldn’t believe it when my test results came back negative. All she could say was to come back in if it got worse. But then what? More tests that didn’t show anything?”
So what happens when you get tested and the test results come back negative for a UTI?
Action To Take When You Get A Negative Test
If your test comes back negative, but you still have symptoms, the conclusion should be that further investigation is needed, NOT that the symptoms are not indicative of an infection.
 | “If a urine dipstick or lab test comes back negative but the patient is clearly describing symptoms of a UTI, doctors must listen to them. Urine tests are far from perfect and it is vital to interpret them in the context of the patient’s symptoms.” |
If your UTI test is negative, it could very well be that the test is wrong.
First, it pays to understand why a test may be negative, despite your symptoms. Discussing this with your doctor will be more fruitful if you know what you’re talking about.
So we’ve gone into this in great detail in our UTI testing section.
Second, you should be aware that medical practitioners rely on guidelines to guide their decisions. Unfortunately, most guidelines used by medical practitioners do not cover the inaccuracies of current UTI testing methods.
This means it is entirely possible your doctor has no knowledge of the issues with standard testing, and may not recommend investigating further. If you’d like to share a reference with your doctor, one set of guidelines that does cover the issues with standard UTI testing is from the American Urogynecological Society.
You know your body. If you have symptoms of a UTI but your test results say otherwise, you have the right to pursue further testing. You can discuss this with your doctor if you feel comfortable doing so.
Alternatively, you can look into private, independent testing; or seek out a practitioner that specializes in chronic urinary tract conditions.
Do I Have Recurrent UTI Or Interstitial Cystitis?
One study found that 74% of females with Interstitial Cystitis had previously been diagnosed with recurrent UTI.
The diagnosis of a single UTI becomes a diagnosis of recurrent UTI once you have experienced at least three UTIs in the last 12 months or at least two within the previous 6 months.
A diagnosis of recurrent UTIs can be indefinite. We’ve interviewed people who have been diagnosed with recurrent UTIs for more than 20 years, with their treatment never changing.
 | “I’m not even sure if the antibiotics are helping, or if it’s just because I drink a bunch of water and it flushes the UTI out. They definitely used to work, but now I think, if my UTIs keep coming back, maybe the antibiotics aren’t really working at all?” |
Some females report a recurrence every time they have sex. Others find it happens when they feel particularly dehydrated, or after intense exercise. And then there are the recurrences that don’t seem linked to anything except time. Some individuals suffer the symptoms of an acute UTI every 4-8 weeks, like clockwork.
In the absence of positive test results, many females will go on to be diagnosed with Interstitial Cystitis (IC). Depending on the knowledge of your medical practitioner and your own research, you may or may not have heard of this term.
 | Interstitial Cystitis is officially defined as “An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes.” |
The last part of that definition is important. It implies that IC can be diagnosed once UTI test results come back negative. That in itself is a little scary.
Can You Test For Interstitial Cystitis?
At a certain point, when UTI tests fail to identify a bacterial cause for symptoms, a diagnosis of recurrent UTI is escalated to IC for many individuals.
We know standard UTI testing methods are inaccurate. So there is a good chance a significant number of people are misdiagnosed with IC after receiving a false-negative on their test results. They may have an infection that testing has simply failed to pick up.
 | “I was told my urine culture was negative, and I therefore didn’t have an infection. I was subsequently diagnosed with IC, but occasionally, during a symptoms flare, I would be culture positive. Eventually I pursued better testing, and found I’d probably had an infection the whole time. I’m slowly recovering, with treatment, and I’m glad I didn’t accept my diagnosis in the end.” |
A number of researchers now believe many cases of Interstitial Cystitis may indeed be caused by bacteria that standard UTI testing has failed to identify.
Read more about Interstitial Cystitis and chronic infection testing and treatment in a dedicated section from our interview with Ruth Kriz.
If you have received inconclusive or negative test results, despite symptoms of a UTI, we encourage you to keep pushing for an answer. Seek better testing and find a practitioner who is willing to work with you.
Antibiotics For UTI And Interstitial Cystitis (IC)
One major difference we see between the diagnosis of recurrent UTI and Interstitial Cystitis is the treatment prescribed.
Females in the recurrent UTI boat are very likely to be prescribed UTI antibiotics for each acute episode, just as they would be for their first ever UTI. This happens whether or not their urine has been tested, and whether or not such testing provides a positive result.
Females diagnosed with IC, on the other hand, are not treated with antibiotics. The guidelines published by the American Urological Association in 2011 do not recommend antibiotic treatment for IC.
 | “I was seeing 3 different doctors for recurrent UTIs, trying to find answers. One diagnosed me with irritable bladder or IC. The other two were still prescribing antibiotics. I had no idea what to do.” |
Given that almost three quarters of females diagnosed with IC were first diagnosed with recurrent UTIs, and that the diagnosis can literally change overnight, there is something obviously wrong here.
One or both of these groups are not receiving appropriate treatment. And it would seem that neither group has access to accurate testing.
Can You Break The UTI Antibiotic Treatment Cycle?
We’ve been chatting to people with recurrent UTIs for a few years now. They’ve helped us map out their treatment experiences. It looks a little something like this – maybe you can find your own story in the flow.

At any point shown in pink, individuals tend to either re-enter the loop, or resort to figuring things out on their own. You’ll also notice that antibiotics appear numerous times in these looped experiences.
Most of our interviewees indicated they have not received conclusive test results, or are not sure if their urine has ever been tested in a lab.
Many have lived with their own sets of chronic symptoms for years. Their experiences are as unique as they are alike.
How To Break The Antibiotic Cycle
Then there are those that break the cycle. And they have some valuable lessons to share. When we asked what allowed them to break free of the infinite loop of UTI antibiotics, these are the insights we heard:
- If you disagree with your doctor’s diagnosis, pursue a second, third or fourth opinion.
- Find a practitioner who understands chronic bladder infection and has shown success in treating patients.
- Take responsibility for your own health, and make the difficult changes you know you should make.
- Don’t look for a band-aid. Seek the root cause of your symptoms, and work with a practitioner that treats the body as a whole.
- Commit to getting well, and remain with your treatment as long as necessary.
- Explore alternative treatments, such as bladder instillations, to address biofilms and directly target organisms.
A big part of the journey to recovery is knowledge. We hope we can help with this.
When it comes to non-antibiotic treatment options, you can learn more about estrogen for UTIs, phage therapy and UTI home remedies, and discuss other potential therapies with your doctor.
We’ve provided information on how chronic urinary tract infection can begin, why you can’t rely on standard UTI testing, and recurrent UTI treatment options, among other topics. We’ll continue to expand our site, and we’d also love to hear from you.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions and comments below, or get in touch with our team.

Hello, I keep trying to post a question but get a message saying ‘Your comment was not posted’. An I doing something wrong. Is there a text limit? Many thanks!
Author
Hi Karen, there is a character limit but it may be that you were experiencing another glitch of some kind. You are welcome to send us any questions by direct message. Melissa
Hi, I am 19 years old and was diagnosed with an UTI, caused by E.Coli (>10^6). They suggested me the following antibioticsFurolin, Fosfocin, Briklin, Netromycin, Ceclor, Zinacef-Zinadol, Procef, Ciproxin, Prixina, Glimbax, Tabrin,
Tavanic, Norocin, Augmentin and Amoxil, Septrin. Which one should I take?? With the least side effects.
Author
Hi Sirene, I saw you also sent us an email so we’ve responded there with more information. Melissa
Grateful for your website and all this info. Looking for a referral for medical professionals you’d recommend in Washington State. Any help you can offer is much appreciated!
Author
Hi Darcy, I saw you also sent an email so I’ve replied there with more information. Melissa
Is there more information and understanding of biofilms and how to treat them? Also – I wish the print on this site was darker and easier to read 🙁
Author
Hi Debi, I just emailed you some more information about biofilms. Feel free to ask any questions there. Thanks for the feedback on the font, I will raise it with our team. We always aim to be as accessible as we can. Melissa
Hello, would it be possible to email me some suggestions for physicians who follow these methods anywhere near Lynchburg, VA? I’ve been desperately looking on my own with zero success and I’m so tired of suffering with a UTI that comes back literally 3 days after the antibiotics run out.
Author
Hi Niki, I just sent you some information by email. I hope it’s helpful. Melissa
Hi, I would like to get info for Physician near me that uses Dr Ruth Kriz’s methods. I live in Dallas Tx. Thank you
Author
Hi Nikki, I just emailed you the info we have on this. Melissa
Like most of us struggling with IC, I’ve seen numerous doctors- urologists, gynecologists, holistic, PTs, etc. I’ve heard many diagnoses- contact dermatitis, urethritis, polyps, OAB, IC, vulvodynia. On top of previous issues with endometriosis, hysterectomy, low/no hormones. I had the embedded infection analysis completed with the following: aerococcus urinae and Viridans group strep. I don’t want to take Levaquin due to side effects, ampicillin made my heart race/dizzy/nauseous. So, now I’m trying doxycycline. Anyone have success with this antibiotic and how long did it take to get results? thanks