Muscles of the Pelvis: Interview with Dr. Bri Grogan
In this video series, Dr. Brianne Grogan, better known as Dr. Bri, shares her top tips on healing and strengthening the muscles of the pelvis. As you may be familiar, maintaining pelvic health can be essential for people with chronic UTI or lower urinary tract symptoms.
Dr. Bri is a leading voice in the field of pelvic health with at-home pelvic floor programs and over 400k YouTube subscribers. She offers a positive and friendly approach to improving your pelvic floor from home.
Dr. Bri’s own experience with pelvic health during and after pregnancy inspired her career in pelvic floor physical therapy. Through Vibrant Pelvic Health and her YouTube channel, she uses dance and movement to help people improve their fitness in a fun and accessible way, while also engaging their pelvic floor.
Using models to help explain the muscles of the pelvis, Dr. Bri describes how they relate to organs such as the bladder. She also provides useful recommendations on how to strengthen these muscles and improve pelvic support, without worsening UTI symptoms.
Browse the summaries of our interview with Dr. Bri or check out our full video interview directly on YouTube. Don’t forget to hit ‘subscribe’ while you’re there.
Jump To Section:
- Anatomy of Muscles of the Pelvis >>>>
- Pelvic Posture is Key >>>>
- Why is it Important to Strengthen Muscles of the Pelvic Floor >>>>
- Pudendal Neuralgia and Muscles of the Pelvis >>>>
- Male Pelvic Floor Function Dysfunction >>>>
- Bladder Retention and the Pelvic Floor >>>>
- At-Home Pelvic Floor Programs >>>>
Anatomy of Muscles of the Pelvis
Using models to explain the muscles of the pelvis in both females and males, Dr. Bri demonstrates the pelvic floor. An outer layer of tiny pelvic floor muscles surrounds the urethra and vagina in females, and the anus in both females and males. There is also an inner layer of pelvic floor muscles that sit more deeply within the pelvic bowl.
During a kegel exercise, involving a squeeze, lift and relax, the tiny outer muscles of the pelvis relate to the squeeze, and the inner muscles relate to the lift. These pelvic floor muscles support the bladder and other pelvic organs like a hammock, sitting at a slightly tilted angle in the body.
Working together with the other muscles of the pelvis, abdomen, back, hips, and diaphragm, they provide balance, stability, and control. They are also important for helping to control the bladder and bowel, allowing things in and out.
What is Pelvic Floor Dysfunction?
Pelvic floor dysfunction is often called chronic pelvic pain syndrome (CPPS). This is a broad umbrella term that covers many things, but essentially indicates that something is amiss with the muscles of the pelvis.
Weakness in the pelvic floor muscles may actually be caused by hyperactivity, where the muscles are too tight to function properly. Pelvic floor dysfunction could also suggest issues with the bladder, bowel, and/or sexual health.
Because it’s often difficult to understand what may be happening in the pelvis, Dr. Bri recommends that anyone facing some kind of pelvic floor issue should try to see a pelvic health specialist. If possible, it would be ideal to see a specialist in person so they can physically examine the muscles of the pelvis.
What is a Prolapse?
A prolapse, or pelvic organ shift, happens when an organ descends or shifts from its usual position. With a bladder prolapse (cystocele), the bladder may shift and press into the front vaginal wall, which may weaken and thin.
It’s a common misconception that a prolapse means the bladder is poking through the vagina. However, a prolapse does not have to be this drastic to cause issues. These shifts toward the wall of the vagina can cause a feeling of pressure and heaviness.
Other types of prolapse may include a uterine prolapse, when the uterus shifts downwards towards the vagina, a vaginal vault prolapse, in people who have had a hysterectomy, or a rectal prolapse, known as a rectocele. A rectocele is when the tissue between the vagina and rectum thins. This thinning may relate to getting older, but could also happen after childbirth or repetitively straining for a bowel movement.
Scar tissue and adhesions may also contribute to prolapse or pelvic organ shift. Dr. Bri uses another useful model to demonstrate how organs, bones, and all the muscles of the pelvis are connected via ligaments and connective tissue called fascia. She explains how soft tissue therapy aimed at releasing or stretching scar tissue can help to move shifted organs back into place.
In severe cases of prolapse, surgery may sometimes be necessary. However, Dr. Bri emphasizes that most of the time non-surgical options like pelvic floor strengthening, vaginal pessaries, and other lifestyle changes can help.
Pelvic Posture is Key
You may have had instances of hunching or curling over to protect your pelvic area when dealing with UTI symptoms. While this “red light reflex” is a natural way for our bodies to react to pain, fear, or stress, it can have a negative impact on posture. Being aware of this positioning is key, as that is the first step in trying to support yourself.
One of the easiest things you can do is alter your breathing. Rather than breathing shallowly up high in your neck, Dr. Bri recommends trying diaphragmatic breathing. To do so, inhale expansively downwards into your ribs and back, and into the muscles of the pelvis.
Another possible postural issue relates to how we sit and stand. People often naturally tuck their butt. But this tucking can tighten the butt cheeks and pelvic floor. As a result, the potential for a prolapse develops.
To avoid this, you can try softening your belly and butt cheeks and ‘blossoming’ out your sitting bones. You’ll have to check out Dr. Bri’s demonstration of how to properly ‘blossom.’
This may not only help release some tension, but this is also good for your posture.
Bladder Safe Working Out
Whether or not it’s a good idea to exercise with chronic UTI symptoms very much depends on you and your symptoms. Dr. Bri explains that with chronic UTIs and chronic pain, your body is run down. Your body is facing both physical and emotional stress, making you unlikely to be in a position to be running a marathon anytime soon. However, this doesn’t mean that exercise is completely off the table.
Many people realize the benefits of exercise for the body and the mind, and are keen to get moving. Dr. Bri supports this, sharing her philosophy that “motion is lotion.” However, she warns that it is important to ease yourself into exercise and micro-dose your movement.
For example, it may be better to do multiple 3-minute walks than one 30-minute walk that flares your symptoms. Because your body is already inflamed, it is going to react more strongly to exercise than if you were feeling your best. It is likely that the muscles of the pelvis will tighten more than they would normally and leave you feeling more sore and painful.
When your body experiences physical and emotional stress, your pelvic floor muscles are some of the first muscles to react. Your bladder may be squeezed, leading to increased UTI symptoms or pressure.
Dr. Bri recommends that people build in at least 5-10 minutes after each workout to completely relax the muscles of the pelvis.
Why is it Important to Strengthen Muscles of the Pelvic Floor?
As with many aspects of health, balance is key. Dr. Bri explains that core-strengthening exercises are best.You can try to incorporate your pelvic floor during these.
Kegel exercises can be useful but they need to be done correctly – with a squeeze, a lift, and a relax. Many people think about the squeeze and lift, but leave out the relaxing part. Kegels provide good training on knowing how to quickly activate your pelvic floor.
Meaghan is one UTI and pelvic floor dysfunction sufferer who has benefited from properly performing kegel exercises. In her story, she also stresses the importance of letting go.
While kegels can be useful, they are an isolated pelvic floor exercise that don’t integrate the rest of the core. We want our pelvic floor to work with the rest of the core to provide balance and control
Exercises that use hip rotation or bring your inner thighs together (adduction) are also great ways to strengthen the muscles of the pelvis. There are several sports that naturally build in these movements, for example horse riding, dancing, and workouts that especially involve the butt/glute muscles.
Pudendal Neuralgia and Muscles of the Pelvis
Out of the many nerves running through the pelvic floor,the pudendal nerve is most commonly referenced within the UTI community. If the pudendal nerve is compressed or irritated, this can lead to pain called pudendal neuralgia.
This pain sensation is felt in the saddle area where your underwear sits, and can make it difficult and painful to sit down. This type of nerve pain may be caused by activities that involve a lot of sitting, for example horse riding and cycling.
If you experience pudendal neuralgia, Dr. Bri recommends that you work on relaxing, releasing and stretching the muscles of the pelvis. If you often sit, try changing up your position, get a standing desk, or take more walking breaks.If your experience is related to sports, such as horse riding or cycling, it may be that you need to take a break. You shouldn’t try to push through the dysfunction because the area needs time to rest and recover.
Activities such as swimming, walking, and some machines at the gym are gentler alternatives that you could try in the meantime. However, you need to be sure that your posture, alignment, and breathing are priority.. Once you have recovered and you feel ready to return to the activity you stopped, take it slowly and build back up over time.
How Can I Strengthen My Pelvic Floor Without Worsening My Hypertonic Pelvic Floor?
Whichever activity you choose, pay attention to how much your core and muscles of the pelvis need to engage. If the exercise requires constant engagement, the muscles will not have an opportunity to relax. This could lead to further pudendal neuralgia issues.
Take extra breaks to relax the pelvic floor. For example, you could try spending around 15 seconds between each movement in a workout to fully release and relax the pelvic floor. Also, don’t forget to build in that extra 5-10 minutes at the end of exercise to focus on relaxing the pelvic floor.
She also suggests focusing firstly on mobility rather than being able to engage the pelvic floor for the entirety of a workout. You can do this through breathing exercises. For example, as you inhale you release the pelvic floor and muscles of the pelvis, and as you exhale you gently lift the pelvic floor and pull in the abs.
In this way, each breath is a mobilization. This technique can also help to get the diaphragm moving, which may become tense and clenched in people with hypertonic pelvic floor muscles.
Which Position is Ideal to Strengthen Muscles of the Pelvis?
How you do your pelvic floor strengthening exercises depends on your level of strength and control of the pelvic floor. Lying down is the best starter position because you aren’t having to fight against gravity. You can also fully relax your body and only focus on your pelvic floor while lying down.
Sitting is the next most accessible option. Your body now needs to fight against gravity, but it doesn’t have to work too hard to keep you upright because a chair provides some support. Most people will find standing during these exercises to be the most challenging because all of your body muscles are working to keep you upright.
It can be a good idea to progressively work up to exercising in a standing position, if possible. Since we spend most of our lives upright, this is the most functional position and it would be great to be able to work your core in this way.
Can I do Kegel Exercises if I Have an Active UTI?
While you can do kegel exercises with an active UTI, you should be careful. Whether you have an acute, recurrent, or chronic UTI, your pelvic floor muscles are probably quite tense. This is because you may be in pain and the muscles of the pelvis are trying to protect you.
You may try to do some kegel exercises and find that you are able to without problems. However, Dr. Bri suggests that it may be best to focus more on breathing and letting go, releasing and stretching your pelvic floor muscles. You could instead try reverse kegels, which are essentially kegels without the lift part.
Male Pelvic Floor Function Dysfunction
While pelvic floor issues may typically be more common in females, this is not always the case. Males may experience rectal prolapse, difficulty with sex, or incontinence issues, which are not uncommon after prostate surgery.
A big issue that Dr. Bri sees with male clients relates to urinary urgency and frequency, and not being able to start the flow of urine. For this, she encourages people to focus firstly on relaxing the muscles of the pelvis. Then, build in more strengthening exercises to help improve coordination and control.
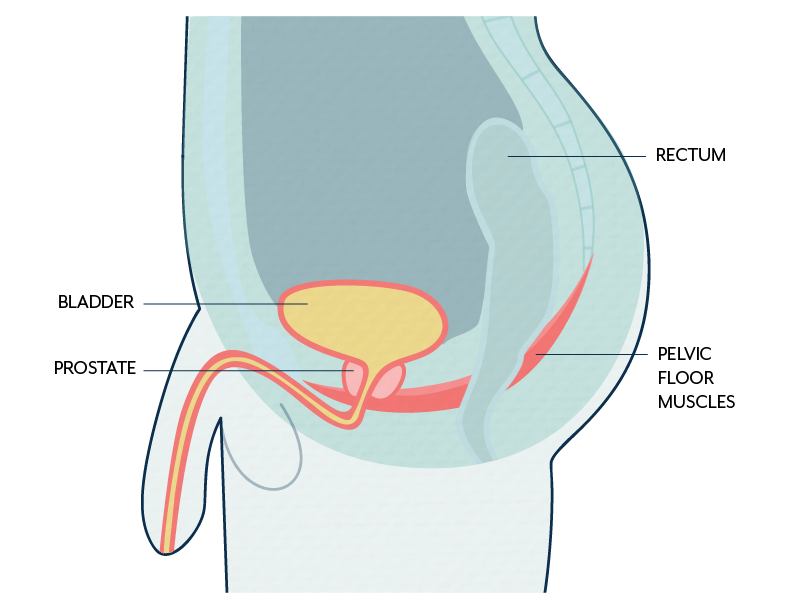
It can be useful to have an internal rectal examination to allow an examiner to feel the muscles of the pelvis and see if there’s pain and/or tension.
There is no obligation to have an internal examination, and an examiner should still be able to gather a good amount of information from an external exam. This would involve feeling the perineum (the area between the genitals and the anus). This is an area where a lot of the superficial muscles meet, with the deeper muscles just above.
How Muscles of the Pelvis Affect the Bowels
Pelvic floor tension could cause abdominal bloating if it makes it harder to open your bowels. Not being able to open your bowels could cause a back-up of waste, which could lead to bloating. General inflammation of the pelvic floor could also lead to abdominal bloating and congestion.
Although bloating can be related to the pelvic floor, there may be something else going on, such as with digestion. Pelvic floor issues are typically multifactorial and interconnected with other things. For example, chronic UTIs and chronic pelvic pain. It could be that you experience bloating because the muscles of the pelvis are too tense, or the muscles of the pelvis might be too tense because you are bloated.
Bladder Retention and the Pelvic Floor
For people with bladder retention caused by prolapse or inflammation, there are methods that can be implemented to help encourage more complete emptying of the bladder. One of Dr. Bri’s favorite things to teach people is the “pelvic rock.”
If you are sitting on the toilet, you can try gently tilting your pelvis forward and letting the muscles of the pelvis settle and relax. Then, you can tilt back and do the same thing, letting your muscles settle and relax.
This technique tips the bladder and the rest of the pelvic organs into a slightly different position, and you might get more out that way. Dr. Bri suggests that once you feel like you have more complete emptying, you can try to do a single kegel exercise. You could do a simple squeeze and lift, hold it for 3-5 seconds and then let go.
It is important to avoid straining while urinating or having a bowel movement as much as possible. Dr. Bri recommends that ideally, you should allow yourself at least 30-45 seconds to let the urine flow out without pushing. If you push hard each time you go, you will be contributing to more downward pressure on your pelvic floor, which could ultimately contribute to prolapse.
How can I overcome the constant need to pee?
Sometimes people feel like their bladder is the size of an acorn. This feeling is likely just a feeling, not a fact. Dr. Bri explains that actually the bladder may have just become overly sensitive to filling. It may be useful to fill out a bladder diary, tracking when and how much you pee (void), and aim to slowly increase the time between voids.
Dr. Bri stresses that this should be a gradual process and you don’t want to suddenly change from going to the toilet every few minutes to forcing yourself to wait hours. Measuring how much you pee may be useful, but not at all required. The main thing is that you try to lengthen the time between each void.
This constant need can be particularly impactful at night and can disturb your sleep. Dr. Bri suggests that sleeping in a position in which you have good alignment can help reduce this impact. For example, sleeping on your side with a pillow between your knees may be helpful.
Bladder leakage and pelvic floor dysfunction
Bladder leakage is usually caused by either physical stress or urinary urgency. Stress incontinence tends to happen when you pee a little bit when laughing, coughing or sneezing. Urge incontinence occurs when you’re rushing to the bathroom and can’t quite make it.
If you’re experiencing these issues, it may be useful to have an examination with a pelvic floor physical therapist. They can determine if the muscles of the pelvis are hypotonic, where they are weak and not working well. It may be that this leakage has been caused naturally through aging or childbirth.
Alternatively, it could be that your muscles are overly tight and therefore squeezing around your bladder and urethra and not coordinated. If this is the case, they may never let go enough to rest and are constantly exhausted.
Some people may experience bladder leakage during sex. Dr. Bri suggests building up your strength over time and remembering to breathe as much as possible. Bearing down could contribute to bladder leakage during sex, too.
With some awareness and control, Dr. Bri explains that you can try to change the contraction that may happen during an orgasm. You could try to intentionally lift the pelvic floor rather than bearing down too much. Evaluation with a specialist can be helpful in determining how to approach and treat these issues.
At-Home Pelvic Floor Programs with Dr. Bri
Dr. Bri has developed a variety of all-encompassing pelvic floor programs that are available at home. Her programs offer a mind-body-spirit approach, as research indicates emotional stress and trauma can impact pelvic health. Each program includes:
- Guided exercises
- Mindset work
- Nutrition adjustments
- An online community
- Lifetime access
Learn more about each program by clicking the program name below:
Overcome Pelvic Pain for Women
Acknowledgements
Our pelvic floor muscles provide our bodies with essential support and stability, and so it’s important that we aim to look after them. However, as Dr. Bri shares, it can be challenging to know what is going on with your pelvic health and how best to do this. If you are experiencing any pelvic health issues, engaging with a pelvic health specialist can be beneficial in helping you navigate them. We want to thank Dr. Bri for taking the time to share her useful insights and recommendations when it comes to pelvic health and UTI.
Subscribe to Live UTI Free on YouTube to watch more expert interviews and to be notified when new videos are released.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions in the comments below, or reach out to our team directly.
