Can Urinary Incontinence Cause UTIs?
What Is Urinary Incontinence?
Urinary incontinence (UI) is defined as the involuntary loss of urine. It’s a real condition, and one that’s much more common than you may realize.
Over 33 million people in the US live with some type of incontinence. It can cause not only physical setbacks, but can also lead to many emotional feelings for those touched by incontinence.
Jump To Section:
- Types Of Urinary Incontinence. >>>>
- Who Does Urinary Incontinence Affect? >>>>
- Impact Of Urinary Incontinence. >>>>
- How Is Urinary Incontinence Linked To UTIs? >>>>
- Treatment Options For Urinary Incontinence. >>>>
- What Can I Do If I Have Urinary Incontinence? >>>>
Types Of Urinary Incontinence
In its simplest form, urinary incontinence is simply not being able to hold urine. But there are actually many different types of urinary incontinence, each with their own causes, and their own treatment options.
Overactive Bladder (OAB)
People with overactive bladder often feel a frequent, urgent need to empty their bladder. This may or may not lead to bladder leakage.
If someone with OAB is unable to make it to a bathroom in time, and an accident does occur (which happens in about half of all OAB cases), the condition is referred to as Urgency Urinary Incontinence (UUI).
OAB is typically caused when there is a coordination problem between the brain and the muscles that control the bladder.
Typically, the brain is signaled when the bladder begins to fill. The brain then signals your bladder muscles to begin contracting, while at the same time relaxing your urethral sphincter muscles.
With OAB, this doesn’t all happen like it should, causing a person to be suddenly aware of a need to get to the toilet.
OAB, sometimes referred to as “spastic bladder”, can often be triggered by specific things, such as hearing running water, or anticipation of needing to use the bathroom.
Stress Urinary Incontinence (SUI)
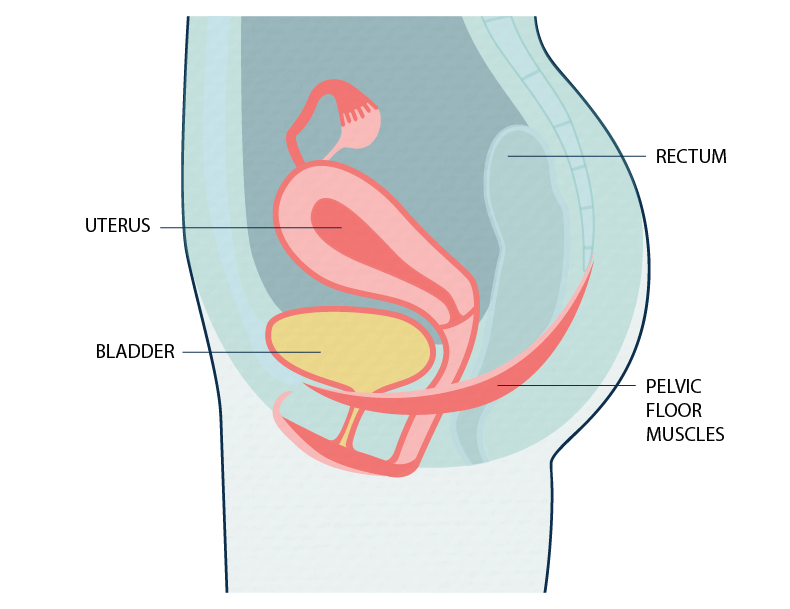
If you have weakened pelvic floor muscles, or a compromised urethral sphincter, you might find yourself with stress urinary incontinence.
This type of incontinence often shows up when pressure is placed on the bladder or pelvic floor. Things like sneezing, jumping, coughing, or laughing can cause unexpected leaks for people with SUI.
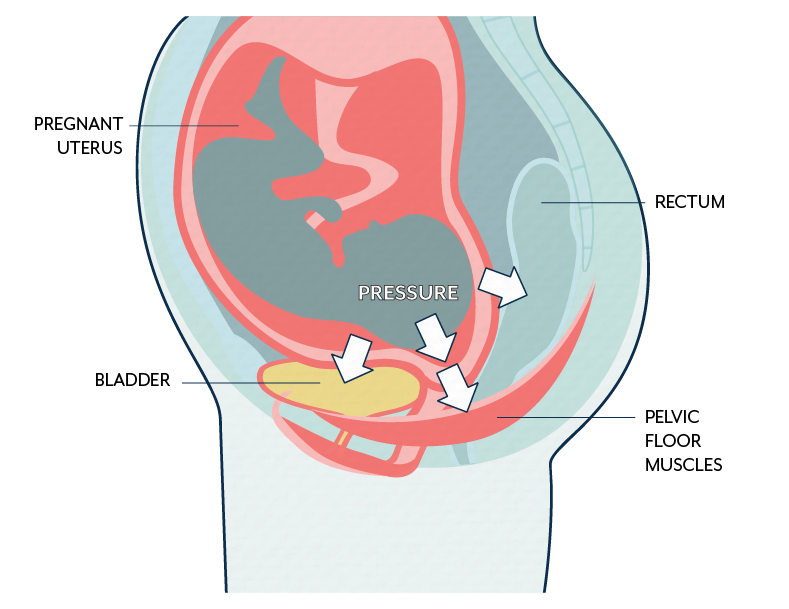
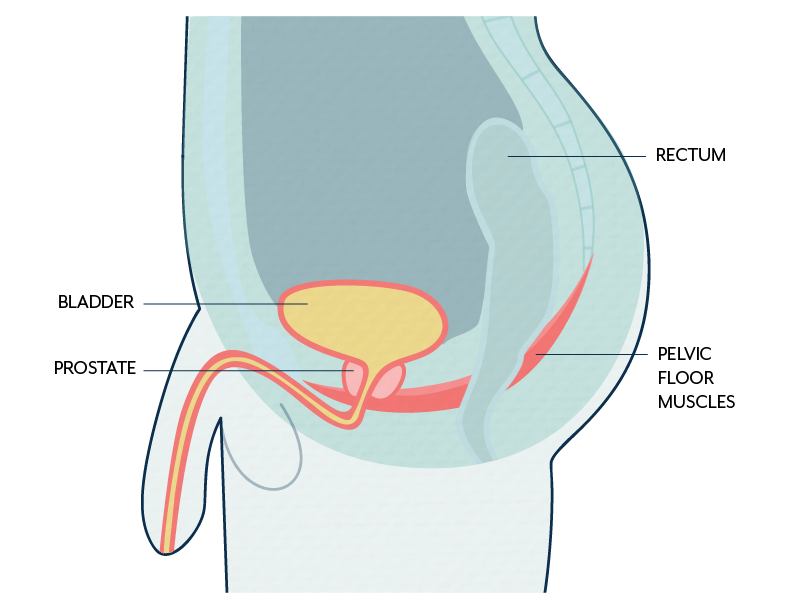
The condition can occur in both males and females. For females, things like pregnancy and childbirth, or menopause can contribute to SUI. For males, prostate cancer treatment, such as a radical prostatectomy, is often the cause of stress urinary incontinence.
Read Carrie’s story, From Nightmare to Healing: My Stress Incontinence Treatment Story, here.
Mixed Incontinence
Some people experience both Overactive Bladder and Stress Urinary Incontinence. This is known as mixed incontinence.
Urinary Retention
People with urinary retention usually have a difficult time starting a stream of urine. They may feel like they need to empty their bladder frequently, even though when they do go, they experience a weak flow, or a need to go again soon after finishing. This can often lead to leakage, since the bladder is constantly full.
Urinary retention is typically caused by either an obstruction in the urinary tract, or nerve problems that interfere with signals between the brain and bladder.
Nocturia
People who find themselves waking more than once a night to use the bathroom may have a condition called nocturia. About 1 in 3 adults over the age of 30 have nocturia, although it tends to occur more as we age.
Nocturia causes us to wake up multiple times at night, disrupting our sleep, which can lead to some serious side effects. The interrupted sleep caused by nocturia can cause real problems with your quality of life and your health.
Many people dealing with nocturia experience fatigue, poor physical function, and decreased cognitive function due to insufficient sleep. Nocturia is also associated with an increased risk for falls (especially worrisome for older adults) and mortality, so it’s a good idea to get it treated.
The causes of nocturia can vary, but it’s most often caused by nocturnal polyuria, a condition where the kidneys produce too much urine. That’s why treating nocturia at the source is so important.
If you’re only focused on treating, say, overactive bladder, you’re only targeting the bladder, not the kidneys. In reality, both conditions should be treated to effectively manage their respective symptoms.
Who Does Urinary Incontinence Affect?
There are many different factors that may lead to one becoming incontinent, though it’s important to note that urinary incontinence can affect anyone; males and females, young and old alike.
The condition is more prevalent in females than males – nearly twice as common. This is partly due to the fact that things like pregnancy, childbirth, and menopause are unique to females and create extra pressure on the bladder and pelvic floor that can cause urinary incontinence.
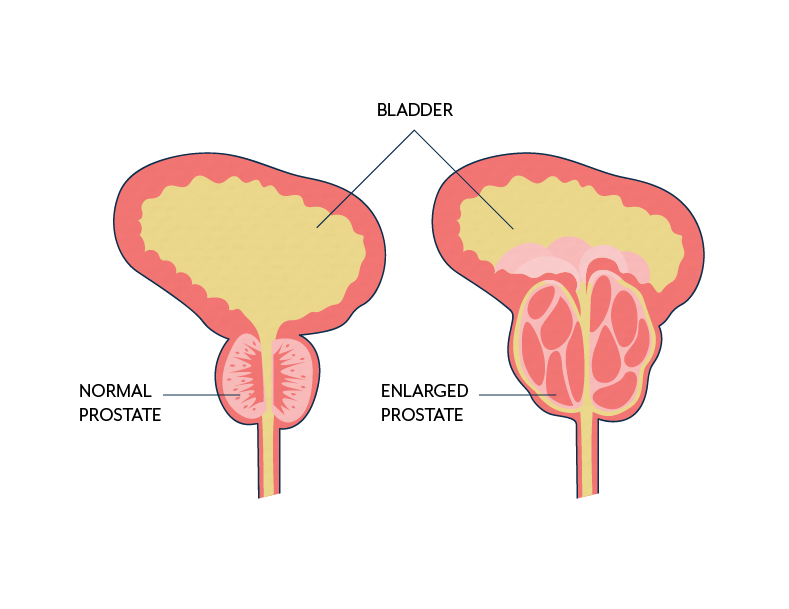
Still, males are not totally off the hook. Issues with the prostate are largely to blame for incontinence in males, especially if the prostate has been removed.
Risk Factors For Urinary Incontinence
Other conditions that can lead to incontinence in both males and females are:
- Other medical conditions, such as diabetes
- Neurological condition such as MS, spinal cord injuries, or Parkinson’s disease
- Being overweight
- Smoking
- Obstructions along the urinary tract that block the flow of urine
- Certain medications
Impact Of Urinary Incontinence
Urinary incontinence is a largely undertreated condition. Despite the widespread prevalence of urinary incontinence, only a fraction of sufferers ever seek treatment.
Issues like stigma and embarrassment keep many from reaching out for help. Yet, despite the unwillingness to talk about it, incontinence is something that greatly impacts the people it affects.
The Physical Impact Of Incontinence
While many people see incontinence as embarrassing, until you’ve experienced it yourself you may not realize the true physical impact that it can have on your life.
Of course there’s the obvious problem of having to change clothes or bedding often, or running to the bathroom, but incontinence can impact your physical health in other ways too. Many people with regular incontinence suffer from skin infections, due to over-exposure to moisture.
Additionally, many people report reducing their physical activity when they have incontinence. For those who were once active, activities such as running or other high impact exercises are often avoided or stopped completely as the practice may lead to unexpected and involuntary leakage of urine.
Finally, incontinence presents a much greater risk for falls and fractures, especially in older adults.
An elderly person who is focused on getting to the restroom quickly may become unaware of the potential hazards that lie in their path to get to the bathroom (especially at night), or may become inattentive to controlling their posture or body movements, which increases the risk of falling.
The Mental Impact Of Urinary Incontinence
While the physical impact of incontinence is substantial, the effect of incontinence on a person’s mental health can be truly devastating. Many people with incontinence carry an emotional burden of shame and embarrassment in addition to the physical disruption on their lives.
They learn to hide their problem from close friends and family, and even significant others for years. They shy away from social activities for fear they will have an accident in public, and stop doing things they once took joy in. Slowly, their isolation and shame may lead to depression and anxiety.
And, the impact doesn’t stop there – sexual function also takes a hit as many females are nervous of leaking during intercourse.
When you think about the anxiety that many feel in relation to possible incontinence during sex, it’s easy to see why many females with incontinence may avoid the act altogether.
The Financial Impact Of Incontinence
As if the cost to a person’s mental and physical health weren’t enough; the economic impact that incontinence has also weighs heavily on patients and caregivers.
Incontinence presents a significant financial burden to the individual and to society. Expenses for things like absorbent products, medications, doctor visits, and dry cleaning or laundry can add up over time. Unfortunately, incontinence gets worse with time if left untreated, and costs only go up as we age.
It’s not just the direct costs that contribute to the financial stress of incontinence. The combination of lost work, plus the funds needed to actually treat the condition can really add up to a financial drain on the pocketbook.
How Is Urinary Incontinence Linked To UTIs?
If you’ve ever had a urinary tract infection you may know that a common symptom is urine leakage. This can be true even for those who don’t normally experience urinary incontinence.
Infections and bacteria within the bladder and urinary tract can cause you to have strong, sudden urges to urinate, which sometimes can result in an accident.
But one thing you may not know is that urinary tract infections are actually more common in people who already experience some types of incontinence. This can be due to several factors:
- People who have a condition that allows urine to build up in the bladder are at risk for developing UTIs because bacteria can build up in the urine that is left in the bladder. These conditions may include:
- Urinary retention
- Prostate troubles
- Nerve damage
- Constipation due to compromised pelvic floor
- Those who use catheters for incontinence may be at a greater risk for UTIs due to the bacteria that can develop if the catheter is not kept clean.
- Poor hygiene habits can cause bacteria to develop around the genital area, which can then creep up into the urinary tract, causing a UTI.
- Many people with incontinence tend to limit fluids to avoid having an accident. However, when this is done to an extreme, it can cause dehydration and a concentration of urine within the bladder, leading to the development of bacteria and infection.
People with urinary incontinence may be able to avoid UTIs by staying hydrated, completely emptying their bladder when they use the bathroom, and practicing good hygiene habits.
Check out our interview with Dr Lindsey Burnett who discusses how incontinence can be connected to recurrent or chronic UTI.
Treatment Options For Urinary Incontinence
Fortunately there are many different treatment options available for those living with urinary incontinence.
Behavioral Modification
Many people with incontinence start treatment by changing up their lifestyle. Sometimes, simply altering what you eat, strengthening your pelvic floor, or retraining your bladder can be the key to staying dry. Some behavioral modifications to try are:
1. Physical Therapy
A physical therapist (PT) can help you locate your pelvic floor muscles and show you the best way to strengthen the muscles. This may involve doing kegels (a common strengthening move) and also other core strengthening exercises (the muscles are all connected, after all!)
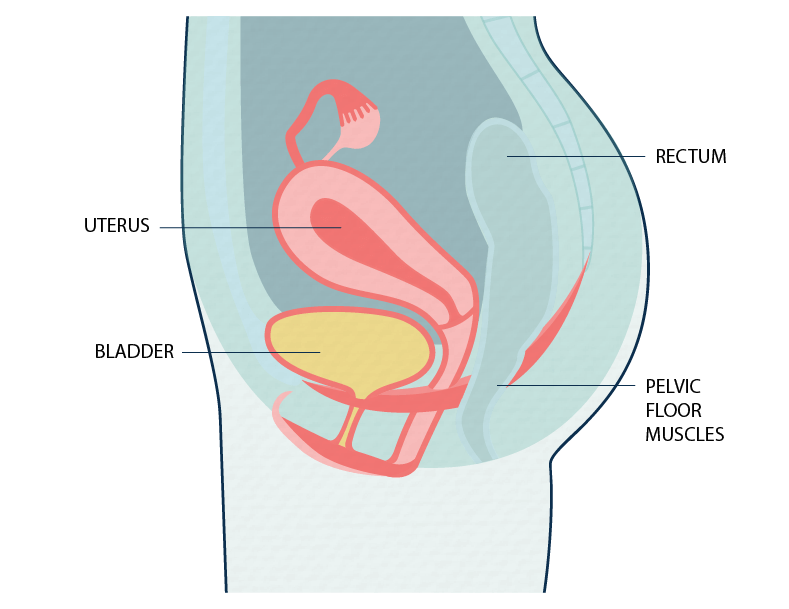
Sometimes, females can also experience a pelvic floor that is too tight, which is just as likely to cause incontinence as a weak pelvic floor. In these instances, a PT will show you how to relax the pelvic floor to allow it to function properly.
It’s very difficult to tell the difference on your own between a weak pelvic floor and a pelvic floor that’s too tight, which is why getting an evaluation by a PT can be so helpful.
2. Biofeedback
Your PT may use a method called biofeedback to measure your pelvic floor strength. There are many different instruments that can be used for biofeedback, but essentially, they measure the muscle activity of the pelvic floor.
A physical therapist will use these measures to coach you in the proper use of the pelvic floor muscles, which can help you improve your strength over time.
3. Diet
Some people experience bladder irritation due to the types of foods they eat. Sensitivities are different for everyone, but some commonly known bladder irritants to avoid are caffeine, spicy food, acidic foods such as citrus or tomatoes, or alcohol.

4. Bladder Retraining
The bladder is a muscle, and just like any other muscle, it can be trained via bladder retraining. By scheduling bathroom times and delaying urination by small increments over time, the bladder can learn to hold urine longer to avoid having an accident, or going so often.
Products For Urinary Incontinence
There are also many products on the market that can help keep you dry – day and night. Some of these are:
Absorbent Products
There’s a world of different types of absorbent products on the market today. Whether you’re looking for light protection or heavy, daytime or nighttime use, pads, or absorbent briefs, disposable or reusable, there’s a product out there for you.
Finding the right one for you can be tricky at first and you may have to try several before finally finding one that fits you properly and works with your lifestyle. But don’t give up. An absorbent product can give you a lot of peace of mind and can help avoid accidents.
Catheters
If your bladder does not empty completely, your doctor may tell you that you need an intermittent self-catheter. Catheters can help improve quality of life by allowing you to completely empty your bladder at regular intervals. This helps protect your kidneys, and lowers the risk of stretching your bladder (because it’s too full).
They’re safe and, once you get the hang of it, easy to use. Both males and females can use catheters.
Pessaries
Many females with a pelvic organ prolapse (POP), a condition that causes the bladder, rectum or uterus to collapse or drop into the vaginal canal, use a pessary for support.
A pessary is a donut shaped device that fits into the vaginal opening and helps support the pelvic floor, providing additional support to the bladder, rectum and uterus. Pessaries can be fitted by a doctor and may prevent the discomfort or incontinence that is often experienced by those with a POP.

Medication For Urinary Incontinence
There are many medications on the market that can treat everything from stress urinary incontinence, overactive bladder, and nocturia, to urinary retention, bedwetting, or BPH. All medications come with pros and cons, so you’ll need to talk to your doctor about what you’re comfortable with.
Advanced Therapies For Urinary Incontinence
If medications don’t work, or you don’t like the side effects that come along with them, there are other options. The procedures listed below can be performed in a doctor’s office, and can provide relief from incontinence.
PTNS/SNM
Percutaneous tibial nerve stimulation, or sacral neuromodulation are two different procedures, but they both work in a similar way. These procedures deliver stimulation to nerves that help to block bladder spasms and can help people who suffer from an overactive bladder. They are low-risk, and non-surgical treatment options that are typically very effective.
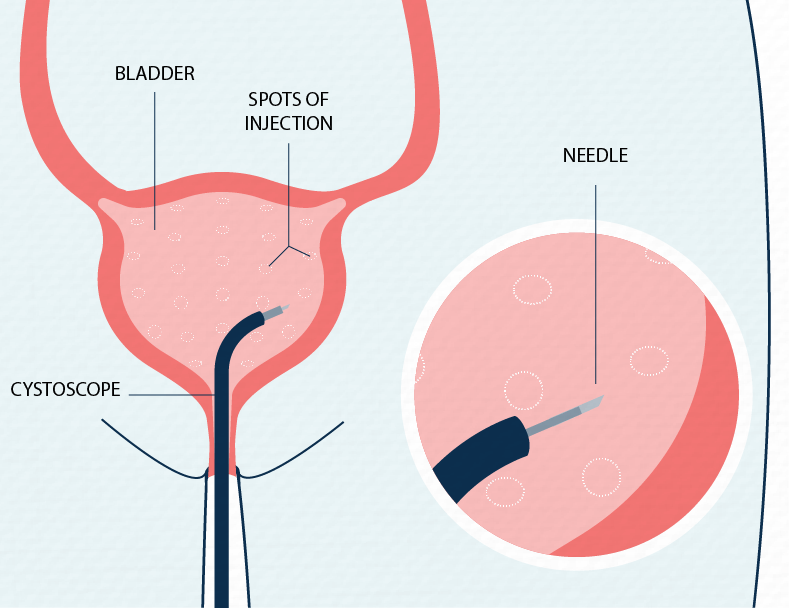
Botox for OAB
You may already know that Botox can be used for wrinkles, but did you know that it’s approved for treating overactive bladder too? Botox injections into the bladder muscle can help block the nerve signals that trigger OAB, reducing and in some cases, completely stopping leakage in patients with OAB.
Surgery
If you feel you’ve tried everything, surgery may be an option for you. There are different types of surgery available for those who live with incontinence, and the type of surgery your doctor suggests will depend on your specific condition. Talk with your doctor about the benefits and risk of surgery to see if this is an option for you.
What Can I Do If I Have Urinary Incontinence?
Your urinary incontinence may have come on slowly, building over the years to the point you now feel you’re ready to treat it. Or, you may have just started experiencing incontinence.
Either way, treatments are available. Incontinence is a condition that is very common, but it’s not normal, and it’s something no one should have to live with.
Here are some first steps you can take to start working toward a treatment plan:
- Educate yourself: Learn all you can about the different types of incontinence and the treatment options available to you. By being informed about your condition, you’ll be better able to have a discussion with your doctor and may be able to better guide your treatment plan.
- Talk to your doctor: This is the biggest step. Having a discussion with your doctor may feel scary or embarrassing at first, but it’s necessary in order to move on to drier days. Your doctor will be able to help you find a treatment option that works specifically for you. Click here for tips on talking to your doctor about incontinence.
- Find support. Sometimes, you just need someone you can talk to that knows what you’re going through. Anonymous message boards can be a huge help for those with incontinence who often feel alone and ashamed to share their condition with those they know. A good message board can help you feel connected with others and can give you the push you need to seek treatment, or even just a place to let out your successes or frustrations.
- NAFC Resources: The National Association For Continence is a non-profit organization dedicated to improving the lives of those touched by incontinence. NAFC.org has many different tools available to you to help you on your journey to becoming dry.
This article was created in collaboration with the National Association for Continence. Visit the NAFC to learn more about urinary incontinence and how to manage it:

