Could An Underlying Bladder Infection Be Causing Your Recurrent UTI?
If you get UTIs frequently you’re most definitely not alone. But did you know recurrent UTIs may actually be caused by a chronic bladder infection that never quite went away?
One in two females will get a UTI in their lifetime, and it’s estimated that up to 44% will have a recurrence of UTI within six months of their first UTI.
And with each recurrence of UTI, the chances of another recurrence increases.
It’s not a great position to be in – with every UTI, you’re more likely to get another, until eventually UTIs become a part of your everyday life. It shouldn’t be that way, and it doesn’t have to be!
UTIs have probably been around as long as humans have had urethras, but long term bladder infections and recurrent UTIs haven’t always been quite so common as they are now.
So when exactly did recurrent UTIs become such a problem?
Jump To Section:
- How UTIs were treated in the past. >>>>
- The difference between chronic and recurrent UTI. >>>>
- Treating a chronic bladder infection. >>>>
- Why your test may be negative, even with infection. >>>>
- Action steps for recurrent UTIs. >>>>
The History Of UTIs Isn’t Pretty
Way back in the 1800s, if you got a UTI, you might be prescribed bedrest, warm herbal compresses, baths, and scarily: opiate-based enemas. It’s also possible that phage therapy was experimented with in some parts of the world.
That was the first round of treatment. If your UTI stuck around, you could expect mustard- or ammonia-based plasters, oral alkali, bleeding (cupping, leeches, or direct bleeding) and large doses of acid solutions.

Not exactly your ideal set of treatment options. And recovery could take up to a few weeks of rest. Interestingly though, it was observed that once recovered, women tended not to have a recurrence of UTI. If you managed to push through, there was a good chance it was a once in a lifetime event.
So why then are recurrent UTIs such an issue these days?
There is plenty of speculation around whether the modern approach to UTIs has actually caused this situation. Rather than expect females to recover without assistance (who wants to spend 4 weeks in bed), antibiotic treatment is initiated early.
While antibiotics generally mean a faster recovery, they don’t allow our bodies to acquire an immunity to the pathogen that caused the UTI. Without the chance to develop an immunity, our body is just as susceptible the next time it’s exposed to the same pathogen.
It is also extremely common for a chronic bladder infection to develop after antibiotic treatment for a UTI fails. This could be because the antibiotics were prescribed too late, or the antibiotics course was too short, or the dosage was too low. It may even be the wrong antibiotic altogether.
When the treatment fails to eradicate the infection, some of the bacteria manage to escape and hide in the bladder lining, forming the foundation of a chronic bladder infection.
This is one part of the puzzle of the growing problem of recurrent UTI, but it’s far from being the only issue. For a brief history of standard urinary cultures, check out our video expert series.
Chronic Bladder Infection Vs. Recurrent UTI
Sometimes, your understanding of a health issue can be muddied by the words used to describe it. Urinary tract infections go by many names, but you’ll often find that everyone is talking about the same thing.
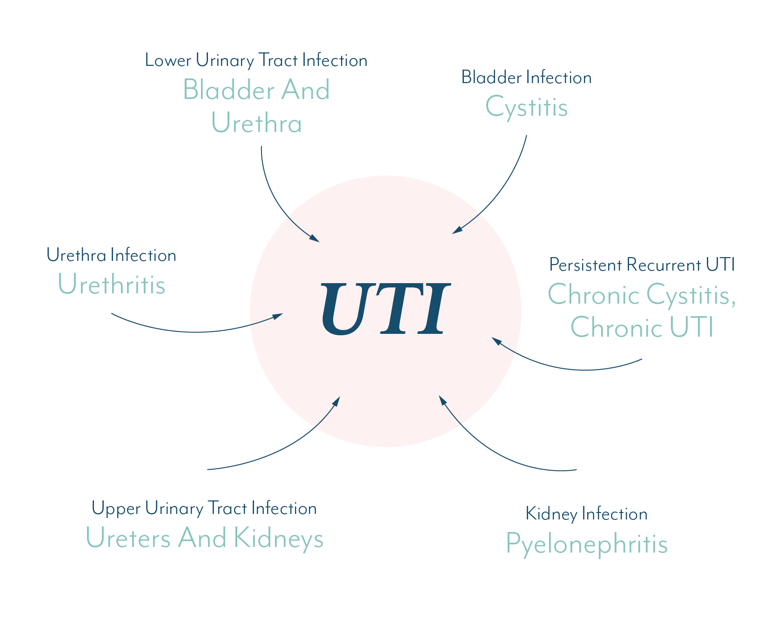
A urinary tract infection can occur in one, or multiple locations in the urinary tract.
Urethritis, cystitis and pyelonephritis are just fancier ways of saying an infection of the urethra, bladder and kidneys, respectively. These are all urinary tract infections.
There is a lot of evidence to suggest that recurrent UTIs may in fact be caused by an infection in the bladder that is not quite cleared by treatment.
A recurrent UTI caused by an ongoing infection that is not cleared by treatment, is called a persistent recurrent UTI.
Persistent can also be referred to as chronic, so the terms ‘chronic cystitis,’ ‘chronic UTI,’ and ‘persistent recurrent UTI’ generally all mean a chronic bladder infection.
Let us further explain how a UTI can become chronic in the first place…
Chronic Bladder Infection Caused By Biofilms
When pathogens first enter the urinary tract, they are free-floating. If given the chance, these pathogens can stick to the bladder lining, and form an intricately linked community, shielded by a slimy layer of protective goop. This slimy goop protects the community from antibiotics, as well as shielding it from the body’s natural defenses.
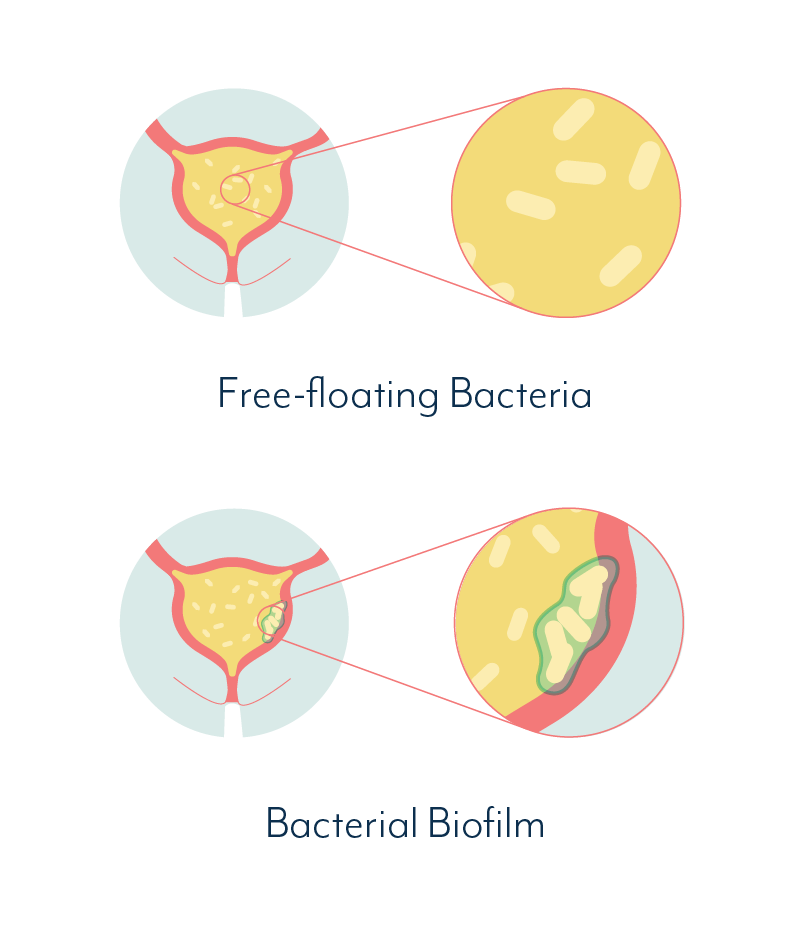
A chronic bladder infection that is attached to, or embedded within the lining of your bladder, is called a biofilm.
You can think of a biofilm as an escalated level of infection; one where a pathogen goes to a lot of trouble to build a resilient community that is in it for the long haul.
Instead of recovering completely from a UTI, your body can be left with an embedded infection that is well adhered to the bladder wall, and isn’t easily moved.
You may get acute symptoms that seem like a new UTI, then periods of minor or non-existent symptoms, before getting acute symptoms again. Then the pattern repeats.
Although this may seem like multiple UTIs, it could actually be part of a cycle caused by an ongoing infection that was never properly treated and flares up at different intervals.
 | “I hadn’t even considered that my recurrent UTIs were actually caused by a bladder infection that never quite went away. But when I think about my recurring symptoms, it makes perfect sense.” |
For those who love to nerd out on science like we do, we’ve provided a more in depth explanation of the fascinating mechanism of biofilms.
Biofilms like those described are thought to be involved in up to 80% of bacterial infections in humans. They are the culprit behind dental plaque, chronic ear infections, stomach ulcers and many other common illnesses.
Up until recently, however, biofilms were not recognized as a contributor to chronic bladder infection.
Fortunately, research is now showing that biofilms can and do exist in the urinary tract, and this research will be extremely important in finding a permanent treatment for recurrent UTIs caused by a chronic bladder infection.
 | “My doctor suspected my constant UTIs were actually stemming from a chronic infection. I was put on longer term treatment and I haven’t had a UTI in nearly two years!” |
Already, thousands of females with long term chronic urinary tract conditions have found better treatment and are now living UTI free. We hope to help even more find a cure.
Treating A Chronic Bladder Infection
Once a bladder infection reaches biofilm stage it can be very hard to treat. For this reason alone, it’s extremely important to treat a UTI early and effectively.
Which brings us to the next problem: It’s not always possible to effectively treat a UTI when we don’t know which pathogen is causing the infection.
Antibiotics for UTI are prescribed on educated guesses, informed by what is the most likely cause of an infection, and which antibiotic is the best known treatment for that likely cause.
When the right antibiotic is prescribed, treatment is often successful. Some research suggests that when the wrong antibiotic is used, or when no treatment is used, it may increase the likelihood of a simple UTI becoming a chronic bladder infection.
So it’s crucial to find the right treatment early.
In order to find the right treatment, it’s essential to know what is causing the infection. Finding the cause can only be done via testing.
When it comes down to it, only testing can provide clear guidance on how to properly treat a UTI and help prevent a chronic bladder infection from forming.
The logical process would be…
Symptoms → Test → Diagnosis → Treatment → Cure
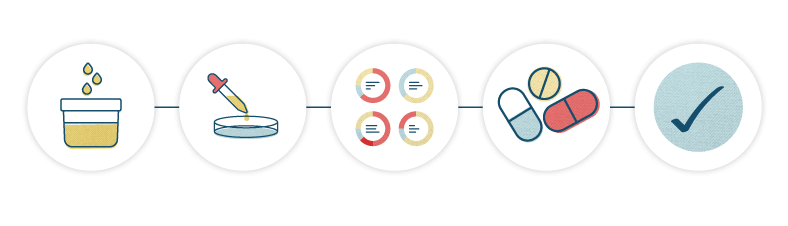
But there is a serious roadblock here: UTI testing is very inaccurate.
You may have experienced this yourself… You show up at a clinic with symptoms of a UTI, and your urine sample is sent to the lab, but the results come back negative.
 | “I had 5 or 6 UTIs in a year, and got tested every time. The results were always negative for bacteria, positive for white blood cells. It didn’t make any sense.” |
Frustrating for sure. But you should know that if this happens to you, there is a very good chance the test is wrong, not your instincts.
And alarmingly, a false negative (when the test comes back negative for infection, but there is actually an infection present) on a urine test often means the infection will be left untreated, and may even get worse.
Why Standard UTI Testing Doesn’t Work
You can’t rely on UTI testing to give you an answer as to what is causing your UTIs. That’s the long and short of it.
Well, that’s the short of it. The long of it goes something like this…
The global standard for UTI testing is based on a couple of studies conducted in the 1950s. These studies focused on women with acute kidney infections and were never intended to be used as the basis for all future testing for lower urinary tract infections.
But, they were. For the last 60 years or so, standard UTI testing has followed the same procedure used in these kidney infection tests from the 1950s.
Quick refresher: a kidney infection is an upper urinary tract infection and can be very serious. The seriousness means the level of bacteria found in the urine is typically high.
Lower urinary tract (bladder and urethra) infections can be caused by much lower levels of bacteria. So testing for a kidney infection may completely miss a lower urinary tract infection.
And that is exactly what happens in up to 50% of standard UTI tests.
That’s right, standard testing for urinary tract infections is inaccurate in up to 50% of cases.
In real terms, that means 1 in 2 UTI tests may come back negative, when there is indeed an infection. You may have been in this position yourself, when you have obvious UTI symptoms, but the test shows you do not have an infection, and your doctor is uncertain on how to proceed.
 | “When all my UTI tests came back negative my doctor prescribed me antibiotics in case it got worse, but said they really didn’t know what else they could do. I felt helpless” |
There are a number of documented reasons behind the failure of UTI testing, and we’ve covered them in more detail in our UTI testing sections.
Where better testing methods have been used for recurrent and chronic UTI, a specific pathogen or multiple pathogens have been identified in an overwhelming number of cases.
 | “My doctor had me submit a urine sample three times a day, taken directly from my bladder with a syringe. She identified bacteria in my morning samples and was able to prescribe the right antibiotic treatment. I haven’t had a UTI ever since.” |
Once a cause is identified you have a much higher chance of successful and permanent treatment. So we’ve also provided some tips on how to get better UTI testing.
We’ve also created a free download that provides a breakdown of the different types of testing. Provide the email address at which you’d like to receive the download, at the end of this article. Or you can jump straight to the download now.
Why Your Doctor Probably Can’t Help With Recurrent UTIs
Medical practitioners rely on guidelines to, well, guide them on how to diagnose and treat illnesses. In some regions doctors are bound by these guidelines and cannot recommend any testing or treatment outside these guidelines.
 | “Most UTI guidelines are aimed at management of simple uncomplicated UTI. It can be very difficult to successfully manage complex or recurrent UTI in primary care. If symptoms persist, or where there is diagnostic uncertainty GP’s will need to make a referral for specialist assessment." |
In other countries, like the USA, medical practitioners can access a range of different guidelines, and can select which they prefer to use as the basis of their practice.
There are pros and cons to both these approaches. In the case of recurrent UTIs and chronic bladder infection there are only cons.
At present there is no set of guidelines for doctors to follow when patients with urinary tract infections do not respond to standard treatment.
No guidelines exist to help clinicians and microbiologists detect and treat biofilm infections of the bladder.
This means there is no mention of chronic bladder infection caused by biofilms, or what steps doctors can take to help their patients before a recurrent UTI becomes a chronic infection.
And there are certainly no guidelines to advise doctors on how to identify an infection once it has become chronic.
Guidelines also fail to provide any information about the inaccuracies of UTI testing, so many practitioners are unaware of this issue.
So although you may show up at a clinic with recurrent UTIs, you are very likely to receive the same testing and treatment as you would if it was your first UTI.
As a patient, you may well have more information about chronic bladder infection than your doctor. Particularly if you’re reading this website.
 | “At some point, after months of unsuccessful antibiotics, my doctor said he didn’t think he could help me anymore. But he also didn’t offer any alternatives. I was on my own.” |
But you can’t blame your doctor for this. Although research has demonstrated that biofilms can form in the bladder and cause chronic bladder infection, the mainstream medical industry is yet to catch up on these findings.
In reality, there are very few practitioners with experience in testing for and treating chronic bladder infection.
So What CAN I Do About My Recurrent UTIs?
As we mentioned above, if you’ve had recurrent UTIs for a long time, it’s possible you have an underlying bladder infection.
Chronic bladder infection caused by biofilms can be very hard to treat, particularly if you don’t know what’s causing it. But finding the cause is tough, given that standard UTI testing is so inaccurate.
 | We know the situation can seem a little daunting, so we have some action steps: |
- Take the UTI Quiz to jump straight to the information you need most.
- Get in touch with us to share your story via a quick interview. Your insight is very valuable to our research and we’d love to hear from you.
- Read the rest of the information in this website, starting with the issues with standard UTI testing. Then do your own research. Understanding the issue is the first step to finding better testing and treatment.
- Take information with you when you speak to your doctor. There’s a good chance they will know less than you do about chronic bladder infections.
- Ask for a referral to a specialist who can help. Or do your own research to find a practitioner with experience treating chronic UTI. Most doctors are unable to assist due to testing and treatment guidelines they must adhere to.
- Request alternative testing or pursue it independently (you have the right to do so in the USA).
- Commit to your health. Change habits that may be making it hard for your urinary tract to heal.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page.

I’ve had considerable difficulty with chronic UTI symptoms and have been unable to find a practitioner who is able to help. Could you send suggestions for a practitioner in the greater Richmond, VA area, or telemedicine options? Thank you and thanks for the work your organization is doing.
Hi Cathy, I’ve sent some information via email. Best wishes, Issy
I’d love information on getting rid of biofilm please. This is my 3rd uti since last summer
Hi Janell, I’ve sent this to you via email. Best wishes, Issy
como combatir biofilm? sospecho de eso dada varias infecciones urinarias mal curadas
Hi Gisela, I’ve sent you an email about this. Best wishes, Issy
Hi, I am based in the U.S. and have chronic UTIs. My doctor has no other solution than antibiotics. Can you please send me more information on getting rid of the biofilms? Thank you!
Hi Christine, I’ve emailed you some information. Let me know if you have any questions, Molly.
Hi can you send me information as well on removing biofilm please? thank you
Author
Hi Court, we got in touch by email and we’re happy to answer any further questions there. Melissa
My 8 year old daughter has been on 3 antibiotics for UTI in the last 3 months and she is still not feeling well. Could you please send me some information on how to remove the biofilms? Thank you!
Author
Hi Magdalena, we sent you some information by email. I hope it’s helpful, Melissa
Hi, I have chronic UTI for 4 years now. Antibiotics only help for a few days. Could you provide me with some information on how to remove biofilms and do you know a specialist based in Germany or a doctor who is offering telemedicine?
Hi Fine, I’m sorry to hear this, I have sent you an email with some resources. Please don’t hesitate to get in touch if you have any questions, Molly.
Hi . I would like to know how to remove the biofilm. Thank you!
Hi Margo, We’ve sent some more information to you via email. Best wishes, Issy