Lower Urinary Tract Symptoms: Is It Really A UTI?
It might come as a surprise that lower urinary tract symptoms may have nothing to do with the urinary tract at all. Or, for many, symptoms of a UTI may have a root cause that contributes to frequent infection but is not an infection itself.
Jump To Section:
- Lower Urinary Tract Symptoms That Could Indicate A UTI >>>>
- When It Is A UTI, But Your Test Is Negative >>>>
- Can STIs Cause UTIs? >>>>
- 5 Common Causes Of Lower Urinary Tract Symptoms >>>>
- 5 Less Common Causes of Lower Urinary Tract Symptoms >>>>
- When To Speak With Your Doctor About Lower Urinary Tract Symptoms >>>>
Here at Live UTI Free, we hear from people on a daily basis who have been diagnosed with a comorbidity (a diagnosis in addition to their primary diagnosis of UTI). We know how important it is to pursue answers beyond infection, as this may be where true resolution lies.
 | "I have dealt with ambiguous, hard-to-identify, lower urinary tract symptoms for years. In the early stages, dipstick tests came back positive and I would get antibiotics, and a few days later the pain would be gone. But, as the pain has continued to linger over the last seven or so years, the doctor’s visits have become less helpful. I started going into the office hoping for a positive test, afraid of the increasingly common outcome of a negative test, a sign I would be sent home yet again without a meaningful solution to the pain." |
While an infection may indeed be present, there are a number of other conditions that could be behind it.
Why Is It Hard To Get A Diagnosis?
Unfortunately, pelvic symptoms can be hard to localize and identify, despite how common they are: Lower urinary tract symptoms occur in 40-60% of women. And once identified, inadequate testing and a lack of research may lead to misdiagnosis, further confounding the problem.
We’ve done some research around 5 of the most common causes of lower urinary tract symptoms (LUTS) and have described them below. It’s important to know that there can be many causes for LUTS, and though this article cannot diagnose you, it may give you an idea on where to start your own investigation.
Lower Urinary Tract Symptoms That Could Indicate A UTI
When suffering with chronic UTI, it’s all too easy to become well acquainted with the tell-tale signs of an oncoming episode. The list below features some of the most common lower urinary tract symptoms associated with UTIs. You can learn more here about how urinary tract symptoms are categorized. Symptoms can vary from person to person or even from infection to infection:
- Urgency – either an almost constant need to pee, or triggered at certain times
- Heightened symptoms at a particular stage of the menstrual cycle
- Incontinence triggered by physical movement (eg exercise, coughing, lifting)
- Inability to empty bladder in a single, strong, continuous stream of urine
- Dysuria – pain related to urination, or just after urination
- Urethral pain, unrelated to urination
- Pain in other parts of the pelvis or abdomen, not specifically the urinary tract
- Hematuria – blood in the urine
- Fever or chills
- Apparent bladder tissue cells in urine (wispy, white pieces)
Of course, each individual experiences the symptoms of a UTI in different ways, so if you suspect you have a UTI, even when your symptoms aren’t ‘classic UTI symptoms’, you should see a doctor.
Not only is it difficult to diagnose LUTS because symptoms can sometimes be a bit vague, hard to pinpoint, or a mix between this and that – many associated diagnoses are equally as vague, hard to pinpoint, and so on.
When It Is A UTI, But Your Test Is Negative
UTIs occur in 40-60% of women at least once in their lifetime, and recur in 26-44% within 6 months. UTIs are widespread enough; they should be able to be clearly identified.
But due to a lack of research, common practice may not always yield the best results. And, unreliable UTI testing means even the tools we do have to identify and solve lower urinary tract symptoms are misleading.
When it comes to causes of LUTS that are less common than UTI, the chance of a true diagnosis may be even worse. This makes it all the more important to know your body well and search for answers of your own.
Can STIs Cause UTIs?
One of the first things many clinicians will ask when a patient presents with recurrent UTI symptoms, is whether the patient has recently been tested for STIs. And rightly so – UTIs and STIs can share similar symptoms, such as pelvic pain, and both can be caused by bacteria. While STIs can also be caused by viruses, like HIV or parasites, all STIs are sexually transmitted.
It’s important to acknowledge that STIs are a major cause of mortality around the world, and can sometimes even present without symptoms. So if you are sexually active you should consider getting tested to protect you and your partner/s.
5 Common Causes Of Lower Urinary Tract Symptoms
We’ve listed five of the most common culprits of lower urinary tract symptoms in order of their prevalence. These are diagnoses you may have received instead of a UTI diagnosis, before or after, or even alongside a UTI. LUTS can come and go, fade into new symptoms, or persist steadily.
Using a journal, or even an app on your phone, may help you track your symptoms. Having more personal data can help an informed physician accurately diagnose the cause of your lower urinary tract symptoms.
It’s important to remember that this list is based on the information available to us, which is limited in its own right.
1. Vaginal Yeast Infection (Vaginal Candidiasis, Vaginal Thrush)
More than 70% of women report having a yeast infection at some point in their life. Around 8% report experiencing recurrent yeast infections.
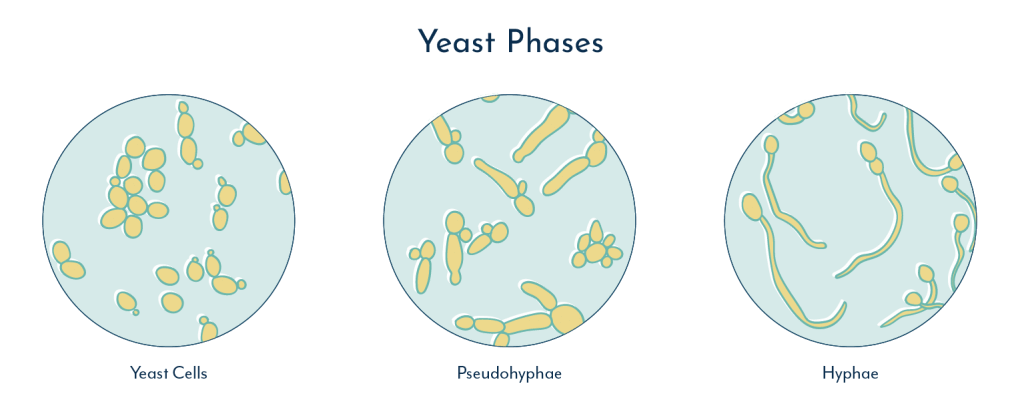
Yeasts, whilst still microorganisms, are not bacteria. They are a subdivision of fungus that can live and multiply as single cells, and are well known for their role in baking bread and brewing beer.
Yeast can also grow by forming connected networks called hyphae, the way other fungi do. When yeast hyphae form in the vagina, it can invade surrounding vaginal tissue causing LUTS.
Yeast in the vagina is usually suppressed by healthy bacteria that both outweigh the yeast in numbers, and produce acids that inhibit yeast growth. However, antibiotics taken for any condition may kill these healthy bacteria and lead to yeast infections of the vagina.
Yeast infection of the vagina is usually caused by Candida overgrowth and the condition is commonly called thrush. Candida cells, which are much larger than bacterial cells and more closely resemble human cells, are thought to be present in the vagina of up to 50% of females at any given time, whilst causing no harm or symptoms.
The lifetime risk of Candida related vaginal infection where symptoms occur, including lower urinary tract symptoms, is 75%.
Symptoms Of Vaginal Thrush
Some of the main symptoms of vaginal thrush are red, inflamed vaginal tissue and the presence of a thick white discharge, often described as appearing like cottage cheese. Sometimes a musty smell is also detectable in vaginal thrush.
The skin of the groin may also be inflamed and appear red and shiny, which can cause a burning sensation. This burning can become much more severe during urination, again mimicking the lower urinary tract symptoms of a UTI.
A vaginal pH of less than 5 is common in people with yeast infections. This may be identifiable with at-home pH dipstick tests.
Recent studies have shown that clinical tests for yeast infections have high sensitivity and specificity, meaning a test by your doctor will likely be able to identify the infection and will allow your doctor to prescribe you the necessary antifungal treatment. If you suspect you have a yeast infection, it’s best to visit your doctor.
2. Bacterial Vaginosis (BV)
Bacterial vaginosis, or BV, refers to when a single species, or a few species of bacteria, become predominant in the vaginal flora. It can be thought of as an overgrowth of these bacteria, altering a normally diverse and balanced bacterial community.
Antibiotics taken for any condition, may, as a side-effect, cause the normal bacterial community in the vagina to change by killing some bacterial species at greater rates than others.
By wiping out some of these bacterial colonies, vacancies are left within the vaginal microbiome which can be exploited by harmful bacterial colonies. As the vagina recovers, problematic bacterial colonies, such as Gardnerella vaginalis, may then disproportionately occupy the vaginal microbiome.
When an unhealthy balance, or dysbiosis, occurs in the vaginal flora, it’s known as bacterial vaginosis. One of the only symptoms experienced by many with BV is a strong fishy odor coming from the vagina.
It has been estimated that the prevalence of bacterial vaginosis in the US is up to 29% in females. Interestingly, around 50% of females with bacterial vaginosis have been found to experience no symptoms at all.
Bacterial vaginosis may, however, cause a burning sensation when passing urine, and this symptom may be incorrectly attributed to a UTI.
Because the vaginal and urinary microbiomes are interconnected, it is also possible that persistent bacterial vaginosis may actually cause recurrent UTIs. Some scientists suspect that a persistently high bacterial count in the vagina may cause a constant seeding of bacteria into the urinary tract due to the close proximity of the urethra.
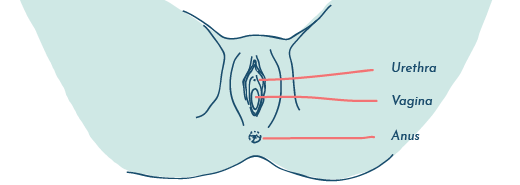
The vagina, urethra and anus are in close proximity
Learn more about UTI and BV in our expert video series.
3. Pelvic Floor Disorders
Pelvic floor disorders are common and may occur in as many as 25% – 37% of adult females.
The pelvic floor is a set of muscles and nerves that support the bladder, uterus, vagina and rectum. Weakness or damage to the pelvic floor may cause fecal or urinary incontinence, constipation, muscle spasms, or a prolapse.
Prolapses occur when pelvic floor weakness allows an organ it normally supports to drop out of place. This can cause the sensation of pressure or heaviness somewhere in the pelvis or genital area.
Pelvic Floor Disorder Prolapses
There are six types of prolapses that are included in the pelvic floor disorders.
- Enterocoele – when a loop of the small bowel slips down between the back of the vagina and the rectum. It may be felt as a heaviness at the perineum.
- Rectocele – where the rectum slips down and protrudes, through the anus, or the rectum is in a collapsed state, lying internally just above the perineum.
- Vaginal prolapse – where the walls of the vagina have slipped down and are lying within or outside of the vulva.
- Uterine prolapse – where the uterus has slipped downward, and lies abnormally low in the vagina. This may be so extensive that the womb lies outside of the vulva completely. Vaginal and uterine prolapse may occur together.
- Cystocele – when the bladder has slipped down between the urethra and the front wall of the vagina
- Urethrocele – when the urethra has slipped down so it is bulging within the vaginal opening or beyond. A Cystourethrocoele is where both bladder and urethra prolapse simultaneously.
The persistence of these systems can cause nerve damage and incomplete bladder emptying, both of which can lead to lower urinary tract symptoms.
Pelvic floor disorders can be risk factors for recurrent UTIs. This may complicate the business of diagnosing the underlying cause of all the lower urinary tract symptoms a patient may be experiencing.
Pelvic floor disorders may be treated with pelvic floor physical therapy, surgery, or a combination of both. Like other muscles, exercises that target the pelvic floor may help correct issues, and in the case of LUTS, may lead to long term relief.
Watch our interview with Dr. Lindsey Burnett who explains the main types of pelvic organ prolapse and the different reasons these might occur.
4. Endometriosis And Lower Urinary Tract Symptoms
The incidence of endometriosis has been estimated to be 10% in adult females. Endometriosis is considered a gynaecological disease where endometrial glands and tissue are found outside the uterus.
While endometriosis may involve tissue growth in pelvic organs, including the ovaries, fallopian tubes, bladder or even urethra, it can also be found outside the pelvis. It may occur on organs such as the lungs and diaphragm, and can occur in the digestive tract.
Although endometriosis consists of tissue similar to that which grows inside the uterus with the menstrual cycle, it is histologically and genetically different. This means its microscopic anatomy and its DNA are dissimilar to endometrial cells that are normally found within the uterus.
There are various theories around why endometriosis occurs, but no consensus. At the very least, research has made it clear that the theory of retrograde menstruation (where menstrual blood ‘flows in the wrong direction’) is incorrect.
Endometriosis In The Urinary Tract
Endometriosis in the urinary tract can lead to recurrent UTI, but it can also directly cause lower urinary tract symptoms, due to inflammatory pain and pressure. Even when the urinary tract itself is not directly involved, endometriosis may cause LUTS.
This is because when endometrial tissue grows in the pelvis, within areas around the vagina, urethra and bladder, it can cause heaviness, and pressure on these structures, often leading to pain.
This pain may be in the form of constant or intermittent symptoms, or dysuria (pain when passing urine). Endometriosis may also be linked to blood in the urine, which would typically be a sign of UTI.
Of the 10% of the female population currently estimated to have endometriosis, 1-6% of these have endometriosis of the urinary tract itself.
Because the presence of endometriosis can increase the risk of recurrent UTI, it’s important to consider other symptoms, as these may be the key to an accurate diagnosis.
Symptoms Of Endometriosis
Symptoms associated with endometriosis include:
- Dysuria – pain or discomfort when passing urine
- Pain passing stools
- Abdominal bloating
- Feeling of fullness
- Dysmenorrhea (painful periods)
- Diarrhea or constipation
- Nausea
- Tiredness
- Difficulty becoming pregnant
- Dyspareunia – pain during sex
- Menorrhagia – excessively heavy periods
- Intermenstrual bleeding – bleeding from the vagina between menstrual periods
For many who experience endometriosis, symptoms can worsen during the menstrual period, but this is not always the case. Symptoms may be present and/or fluctuate at any point during the cycle.
Endometriosis is extremely underdiagnosed, with the average time to diagnosis between 7-9 years, depending on the country.
For this reason, if you feel your symptoms may warrant further investigation, it’s important to find a specialist that works with other endometriosis patients. Most clinicians are not equipped to make a diagnosis of this type.
5. Vulvodynia
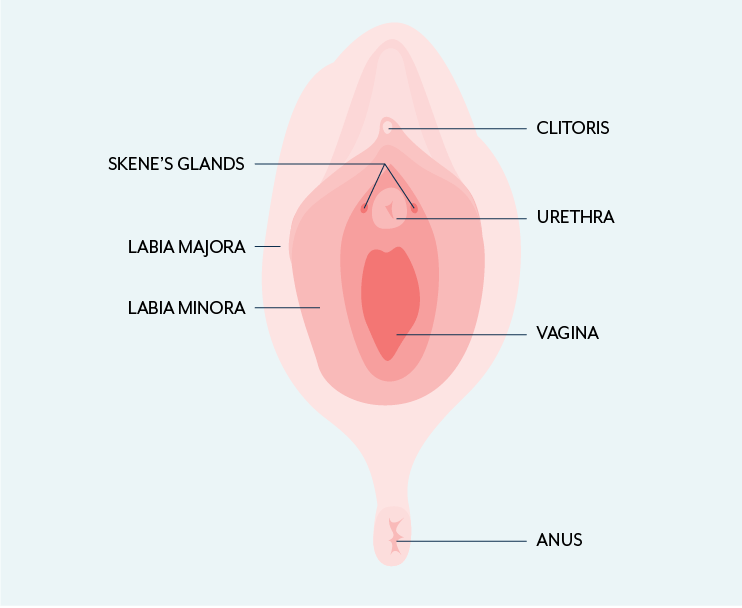
Vulvodynia is a disorder of pain involving either much of the vulva or specific parts of the vulva, i.e., the clitoris, labia or entrance to the vagina. The disorder was estimated to be prevalent in 8.3% of the female population of Michigan, USA. We could extrapolate this figure to the rest of the USA, however, specific numbers are not available.
When different areas of the vulva undergo pain it is termed Generalized Vulvodynia. When only a specific area of the vulva is affected it is called Localized vulvodynia.
Generalized Vuvlodynia can be constant or intermittent. It may be provoked by direct pressure, and this may make the pain worse, though neither are necessarily true.
Localized Vulvodynia is more typically a burning pain that is present in a specific area of the vulva. Direct pressure during sex, bike or horse riding, or even sitting at a desk for work, can bring the pain on and/or aggravate it.
Because vulvodynia can present similarly to other conditions, a record of symptoms – i.e., when they occurred, what made them better, what made them worse, how long they lasted – can be crucial in ruling out other conditions and determining the appropriate diagnoses.
Vulvodynia is characterized by a burning or stinging sensation, as though the vulva has come into direct contact with an irritant. Take note of the character of the pain, as well as the washing products you use for yourself and your clothes.
Consider whether any normal activities seem to trigger the pain or make it worse. These could be as simple as washing/showering, sex, tampon insertion, physical exercise, or direct pressure to the vulva. It’s also important to note where exactly the pain occurs.
Watch Dr. Maria Uloko’s interview in which she discusses vulvodynia and other pelvic pain here.
5 Less Common Causes of Lower Urinary Tract Symptoms
1. Skenitis (Female Prostatitis)
Around the lower end of the urethra are the Skene’s glands, also known as the paraurethral glands. These glands are the female version of the prostate gland and they’re usually rather unnoticeable.
Bacteria in the vagina can block the Skene’s gland causing a build up of pus and the formation of a cyst, which can then cause lower urinary tract symptoms such as:
- Dysuria (pain while urinating)
- Dyspareunia (pain before, after, or during sex)
- Inability to empty bladder
- Vaginal discharge
Additionally, skenitis can cause recurrent urinary tract infections, as bacteria may continually be seeded into the urethra.
Skenitis is considered to be rare, however, no real data exists around how common it is. Research has shown that skenitis may be more common in females in their 30s and 40s.
Cysts associated with skenitis are often large enough to be felt during examination and sometimes even produce pus when squeezed. Skenitis is typically treated surgically by draining the cyst and with the use of antibiotics.
2. Urethral Diverticulum
Skene’s glands can also become dilated, which is thought to be the most common cause of urethral diverticulum (UD), a pouch that forms in the urethra. However, UD can also be caused by a birth defect or trauma during childbirth.
The lower urinary tract symptoms associated with UD include
- Pelvic pain
- Blood in the urine
- Incontinence
- Pain during sex
Urethral diverticulum can also cause recurrent UTIs.
Population based studies have found 6 – 20 UD cases in 1 million women, making it fairly uncommon. This comes with the caveat that the Urology Care Foundation has found that UD is often first misdiagnosed.
Proper diagnosis can involve imaging, like an MRI or ultrasound, detailed health history, physical exams, and urine analysis.
Luckily, once diagnosed, treatment for UD can help resolve LUTS. Surgery to treat UD has been found to be 90% effective, with low rates of recurrence.
3. Ureterocele
Swelling at the bottom of a ureter, known as a ureterocele, can cause the back flow of urine from the bladder into the kidney.
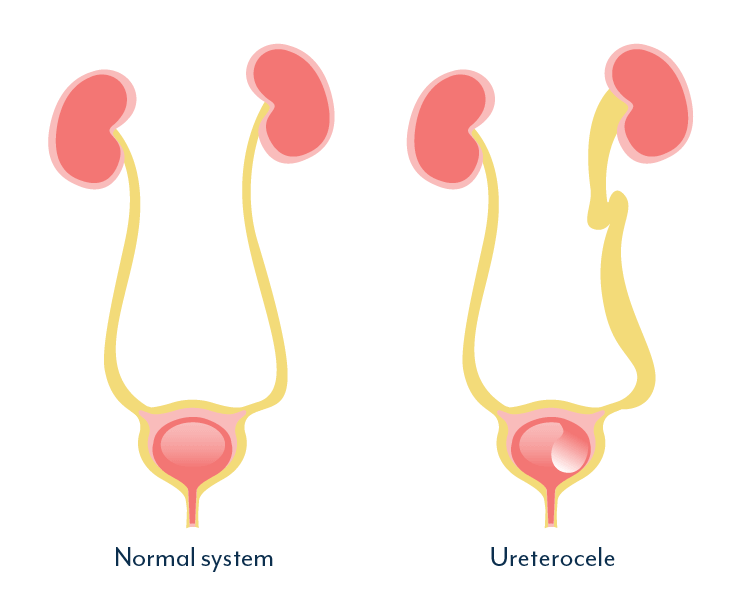
Occurring in 1 in 500 people, ureteroceles are most commonly recognized as birth defects, with the possibility that the disorder runs in families. However, studies have also shown that ureteroceles may develop in adults.
Ureteroceles can cause common lower urinary tract symptoms such as dysuria, hematuria, urgency and frequency, as well as UTIs. Fortunately, ureteroceles can be easily diagnosed with imaging and treated with minimally invasive surgical methods.
4. Bladder Cancer And Lower Urinary Tract Symptoms
The average rate of bladder cancer each year is 20 cases per 100,000 people, with the average age of diagnosis being 73 years old.
Bladder cancer causes many lower urinary tract symptoms such as urgency, hematuria, burning and dysuria. There are many tests to identify bladder cancer, including urine tumor marker tests, biopsies, and urine analysis, among others.
There are various options for bladder cancer, including surgery, radiation, and chemotherapy, dependent on the stage of cancer and other factors.
Bladder cancer treatments are relatively successful, with a 76.9% 5 year survival rate.
5. Chemical Sensitivities (Genital Contact Allergies)
Specific brands of condoms, soaps, lube, douches, cosmetics, and natural occurrences like sweat, discharge, or urine can cause adverse reactions.
 | "Chemical sensitivities is a condition that is close to my heart, because ever since a young age I have had sensitive skin. Lotions would give me rashes, certain detergents gave me eczema, and so on." |
Genital contact allergies can cause burning while urinating, itching and irritation, swelling, and other common lower urinary tract symptoms. Therefore, keeping a track of your symptoms may allow you to identify whether a particular chemical sensitivity is causing your LUTS.
One small study found 39% of participants had some form of genital allergy, but genital contact allergies on a large scale are frequently missed.
If you think you may have a particular sensitivity, you should speak with your doctor.
Wrap Up Of Other Causes We Didn’t Cover
Of course, human biology is complicated. In many ways it seems it may be easier for any one thing to go wrong, than to be lucky enough for everything to go right. Lower urinary tract symptoms can be caused by different conditions at different times, or even by different conditions at the same time.
This list doesn’t comprise every possible cause of LUTS. That would be impossible. For example, menopause, kidney reflux, or kidney stones may also cause LUTS. Other diagnoses are more controversial, and with unreliable tests and the lack of research, it may be some time before we learn any real answers.
When To Speak With Your Doctor About Lower Urinary Tract Symptoms
Tracking your symptoms is crucial to finding valid, reliable, and treatable causes for LUTS. The National Association for Continence suggests keeping a diary for at least 4 days, but a week is even better.
As mentioned earlier, there are apps for chronic pain tracking that allow you to identify the types of pain and its location and take notes.
It cannot be overstated how important it is to have a doctor willing to enter the battle with you. You need someone on your side when nothing seems to be working – a physician you trust will keep fighting for you.
Finding the right clinician can be tough. We may be able to help, so send us a message if you’d like more information.
Even with the right doctor, LUTS are personal and often uncomfortable. It can be hard to stand up for your best interests when it includes putting your pain out on the table for your doctor to analyze. Being honest and direct with yourself and your doctor can help solve some communication issues.
And don’t be afraid to bring in backup. Taking a supportive friend or family member can help alleviate the stress and remind you that you are not going through this alone.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions and comments below, or get in touch with our team.

Hi, I was prescribed 7 days Lexoflaxin for acinobacter and it didn’t help. Tried cranberry, drank gallons of water and everything else I have seen online. Nothing works. 3 weeks now. Not sure if u have any suggestions to this. Thanks in advance.
Hi Sarah, can you please send me a direct message and let me know where you’re based so I can share the most appropriate information? Melissa