Professor Malone-Lee on Chronic UTI Treatment
What are the differences between chronic and recurrent UTI? Is bacterial identification the only way to diagnose and treat an infection? What about sex? How does sex impact a UTI and vice versa?
These are some of the common questions we receive, so we passed them along to someone who could help answer them, Professor James Malone-Lee. Professor Malone-Lee passed away in early 2022 and we were grateful to have a chance to receive his insights.
Professor Malone-Lee was one of the researchers and clinicians exploring these questions and more while treating patients with chronic UTI. As is the case in many areas of science, much information has been gained, but there is always more to learn and explore.
During our interview with the professor, he provided us insight into how he diagnoses and treats chronic and recurrent UTI. His method primarily includes plotting patient symptoms, white blood cell, and epithelial cell counts on a graph to monitor patient progress. Patient symptoms are the focus of his treatment protocol and are measured throughout to determine progress.
Professor Malone-Lee had an entertaining way of sharing this information. So catch up on the video interview below or on our YouTube channel to hear all the details, or browse the included summaries.
Jump To Section:
- Recurrent vs. Chronic UTI >>>>
- Diagnosis And Long Term Treatment >>>>
- UTI Recovery And Specific Organisms >>>>
- Sex, Fertility, And Antibiotic Side Effects >>>>
- Imaging And How To Talk With Your Doctor >>>>
Recurrent vs. Chronic UTI
We understand the limitations of standard urological tests today, but Professor Malone-Lee first began to recognize these shortcomings back in the 1990’s. He observed that the urodynamics tests were not aligning with patients’ reported symptoms, and later noticed that cultures were not supporting evidence of infection that appeared on dipsticks.

Once the limitations of dipsticks were also confirmed, he transitioned to using a microscope to evaluate the state of the bladder. He gradually began to treat patients with overactive bladder symptoms (OAB) as though they had a urinary tract infection. To his satisfaction, patients improved while treating with antibiotics, and he was able to work with a team of Phd students to perform more formalized research.
One of the symptom traits Professor Malone-Lee recognized, was the ‘quirky’ symptoms patients reported. These symptoms were outside the widely accepted list of UTI symptoms, but nonetheless, those symptoms would improve through antibiotic treatment.
As Professor Malone-Lee explained, “biology does not exist in categories,” and when it comes to persistent lower urinary tract symptoms (LUTS), the UTI exists on a spectrum. The UTI spectrum begins with an acute UTI, contains various patterns for individual patients in the middle, and ends with chronic symptoms on the other end.
He points out that these organisms have had millions of years to evolve, and because of their sophistication, they have developed specific methods of attacking the human body. Some bacteria can cause inflammation by invading the tissues, while others burrow into cells and become dormant. When the dormant bacteria are forced to relocate due to the natural shedding of the bladder tissues, they can cause acute symptoms as they move from one cell to another.
For patients who have constant symptoms, Professor Malone-Lee attributed that to a chronic low level immune response rather than specific organisms.
Diagnosis And Long Term Treatment
When it comes to diagnosing a chronic or recurrent UTI, Professor Malone-Lee relied primarily on symptoms. Performing a microscopic analysis of a patient’s fresh urine sample provides support for the diagnosis. However, because of the disintegration of cells, the amount of white blood cells (WBC) decreases by approximately 60% within two hours, so their specific count is unreliable for a diagnosis.
Another type of cell that is considered in the urine analysis is epithelial cells. Epithelial cells (or cells from tissues of the body) in the urine are cells that makeup the tissues of the bladder. Once believed to be contamination, epithelial cells are now recognized as part of a UTI within the professor’s clinic. Through his team’s research efforts, they identified a pattern of excess epithelial cells in the urine of symptomatic patients, as compared to asymptomatic people.
Rather than using WBC and epithelial cell counts to diagnose an infection, the professor uses the cell counts to plot a graph and track the course of the infection through treatment. This has allowed his team to cut down on the amount of antibiotic changes when patients report an increase in symptoms.
If a patient’s graph is demonstrating that the infection is improving, he advises the patient to maintain the current treatment. Using this approach, the symptoms typically improve as the graph pattern predicted.
In addition to first line, narrow-spectrum antibiotics, Professor Malone-Lee also recommended Hiprex (Methenamine) as part of a treatment protocol. Hiprex works by acidifying the urine and producing formaldehyde within the bladder. As a result, it works as an antiseptic and bacteria are unable to multiply.
A group of patients who are unable to tolerate antibiotics use Hiprex only to treat their UTI. The progress is slower because bacteria are not being directly targeted, but are restricted in their reproduction.
UTI Recovery And Specific Organisms
The journey to complete healing from a chronic or recurrent UTI is often met with highs and lows. Sometimes a cause as to why either occurs is not identified. Although it is typical for patients with a UTI to not have a consistent improvement in symptoms, Professor Malone-Lee focused on the cell counts and graphs to determine if overall progress is being made.
The term for these highs and lows with an overall improvement is damped oscillation. The WBC and epithelial cell counts may have many peaks and valleys throughout treatment, but as long as the peaks become lower as treatment progresses, the professor considers the overall trend a positive sign.
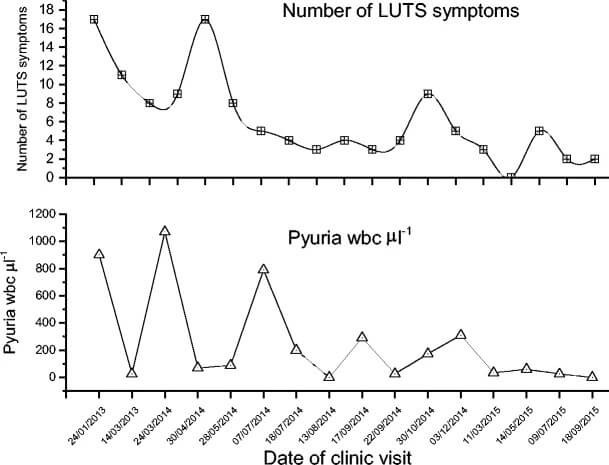
It’s common for patients to experience symptom flares throughout treatment, and when they arise they can be quite discouraging. But as long as damped oscillation is taking place, Professor Malone-Lee believed the current treatment is appropriate and the symptoms will calm down over time.
The limitations of standard urine cultures are well documented, so the professor does not currently use any diagnostic tests to identify specific organisms. While organism identification tests are not used, his team has observed a relationship between a group of patients who responds well to a specific class of antibiotics.
Based on these observations, they believe obligate intracellular microbial infections may be at the root of this group of patient’s symptoms. Obligate intracellular microbes include Mycoplasma, Ureaplasma, Chlamydia, and Legionella.
As far as determining if certain organisms may be responsible for specific symptoms, Professor Malone-Lee had plans to begin a long-term research project aimed at investigating this further.
Research has also shown that certain organisms may be associated with particular symptoms for male patients experiencing chronic prostatitis.
Sex, Fertility, And Antibiotic Side Effects
Many patients with chronic or recurrent UTI report an increase in LUTS during or following sex. During sex, pressures in the pelvic area can disrupt the cells of the bladder. While uncomfortable or painful, this process and post-sex symptom flare can provide insight into the effectiveness of treatment.
While it’s not necessary to engage in sex during treatment, Professor Malone-Lee’s team recognizes the impact of sex on symptoms. The improved response to sex over time can be a valuable tool in measuring treatment progress.
 | “If you perturb the cells, the bugs that are colonizing those cells will get a fright. They'll wake up, start dividing. I mean if you give a bug a fright, it'll just start dividing. That's all they do. That's their one reaction to adversity - divide. And as a result they produce a whole lot of progeny that then burst out and charge for safety.” |
For Professor Malone-Lee’s patients, he recommended a temporary increase of antibiotics around the time of sex to prepare for the excess activity of bacteria. Typically, as his female patients continue with treatment and having sex, they’ll notice their symptoms following sex become less severe.

Another connection the professor has made is the occurrence of his patients becoming pregnant during treatment after previously struggling with infertility. An infection can increase the risk of miscarriage, premature birth, and preeclampsia, but can UTI impact fertility as well? Without further research, we can only consider theories.
During pregnancy, women begin to shed epithelial cells in an excessive manner. This may be due to the body’s innate way of protecting the woman and child from infections during pregnancy. Because the shedding of epithelial cells helps to rid the body of bacteria, this process may also be contributing to decreased risk of poor pregnancy outcomes as well.
Imaging And How To Talk With Your Doctor
Aside from using microscopy results to track patient progress through treatment, Professor Malone-Lee used other various diagnostic tools. Every patient who comes under his care receives a renal tract ultrasound to check for stones. Ultrasound is also used if a patient is not progressing in their care, to determine if stones formed along the way.
Both urine cytology (which checks for abnormal cells) and a cystoscopy are performed for patients experiencing blood in their urine. This simple workup is considered effective for ruling out polyps or pre-cancerous growths.
Hunner’s lesions are seen during cystoscopy for some of the professor’s patients. While some people with LUTS receive a diagnosis of interstitial cystitis (IC) based on the presence of Hunner’s lesions, it’s important to keep in mind that IC is a diagnosis of exclusion. The history of Hunner’s lesions shed lights on their structure being identical to ulcerations caused by cystitis, or bladder inflammation.
Many of Professor Malone-Lee’s patients had received a diagnosis of IC in the past. Although they may have Hunner’s lesions, the professor has not observed a difference in the treatment response of IC patients vs non-IC patients.
The concepts discussed with Professor Malone-Lee are fairly simple, however, some patients have difficulty discussing them with their own clinician. When these discussions become difficult, the professor recommends raising a question to your physician as a way to encourage them to consider a UTI as a cause of urinary tract symptoms. After presenting evidence of chronic LUTS and the limitations of standard cultures, respectfully ask your physician how it is best to proceed with your care, given this information.
“Listen to your patient, [they are] telling you the diagnosis.”
Dr. William Osler
If you’ve found this information helpful, you can support future expert interviews and other projects by contributing to the work that means the most to you. To become more actively involved, become an official Live UTI Free member.
Acknowledgements
Many approaches to treating chronic and recurrent UTI are used by professionals in the UTI community. For Professor Malone-Lee, a simple, straightforward approach to both diagnostics and treatment was effective for his patients. When it comes to UTI during pregnancy and attributing specific organisms to specific symptoms, additional research is needed. We are grateful to the professor for sitting down with us and giving our community insight into his treatment methods and ongoing research.
As a reminder, Live UTI Free does not endorse a specific approach to treating chronic or recurrent UTI.
Subscribe to Live UTI Free on YouTube to watch more expert interviews and be notified when new videos are released.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions in the comments below, or reach out to our team directly.

Hi i’ve been told i have sensory urgency. Had a cystoscopy and uridynamic testing,so told its not OAB. I use vagifem x2 weekly and been prescribed Solifenacin. Is there anything else i can do or take. I am 64 yrs old
Hi Gill, can you please send me a direct message and let me know where you are based? I will share any relevant resources we have. Melissa
Hi Melissa, i live just outside Portsmouth Hampshire
Gill
Thanks Gill. I just sent you an email with more information. Melissa
I keep getting a uti I’ve had this one for a month and antibiotics not working and urine clear doctor says I’m coming resist to antibiotics and doesn’t want to giv me anymore what do I do
Hi Margaret, sorry to hear you’re experiencing that. Are you able to send me a direct message and let me know where you’re based? I’ll share any resources that are relevant. Melissa
Over the last few years I have had pain and the feeling like something is about to burst around my bladder area. I am on long term antibiotics. In May this year 2021 I started to take bio identicals with an estrogen gel and Ovestin vaginal. At 65 this gave me a period in June which I was expecting but a few days later I felt blood gushing intermittently from my urethra as well. I made sure of this before seeing a doctor at A and E but because the doctor had no diagnosis she tried to convince me the blood wasn’t coming from where I said and know it was.
I have had cat scan with nothing showing up from the kidneys but did show some fluid in the endometrium. I have had cystoscopy when not bleeding and this was normal. But the girl did say there was a bulge outside of the bladder.
Hi Valerie, it’s important to speak with a specialist about this as these types of symptoms should be investigated. I’m not sure where you are based so I’ll send you an email as well. Melissa