Dr. Hlavinka On Recurrent UTI and Hormones, Sex, And Interstitial Cystitis
Dr. Hlavinka sat down with us to discuss some areas of health that can impact chronic or recurrent UTI. In our video interview, we touched on a range of topics surrounding UTI, including hormones, sex and the often considered link with interstitial cystitis (IC).
Dr. Tim Hlavinka also provided a unique insight into the relationship between female health and UTI, and how sexual partners may impact bladder health.
Watch the videos below or read each transcript by clicking on the included link.
Jump To Section:
- Dr. Hlavinka Discusses UTI and Hormones, HRT, and Contraceptive Methods >>>>
- Probiotics, Biofilms, and Interstitial Cystitis With Dr. Hlavinka >>>>
- How Is Interstitial Cystitis Diagnosed? >>>>
- New Treatments For Interstitial Cystitis, UTI, and Prostatitis >>>>
- UTI And Sex: Should I get My Partner Tested? >>>>
- UTI And BV, Yeast Infection And Other Risk Factors >>>>
Dr. Hlavinka Discusses UTI and Hormones, HRT, and Contraceptive Methods
According to Dr. Hlavinka, there is an undeniable link between hormones and bladder health in women. During hormonal milestones, such as puberty, becoming sexually active, becoming pregnant, and both peri and post menopause, women are at increased risk of infection.
Sometimes these milestones contribute to hormonal deficiencies, but the potential for hormonal imbalances and fluctuations without deficiency also exists. This is seen often during breastfeeding periods, for instance.
Dr. Hlavinka also sees perimenopause as a time that comes with an increased risk of infection, and he’s experienced a concerning increase of female patients in early perimenopause. It’s become common practice to place perimenopause patients on hormone replacement therapy (HRT). However, oral hormones can diminish estrogen levels and lead to early menopause. A now recognized genetic mutation on the androgen, places 7% of women at risk of premature menopause due to contraceptive use. As little as six months on a low-dose pill increases these risks.
For people who are menstruating and not on birth control, there are two times during their cycle that they are at increased risk of infection. After menstrual bleeding ends, there is an increased risk of infection due to the decrease of hormones.
Pre-ovulation and ovulation, while a time of tissue protection due to surging levels of testosterone and estrogen, also have an increased risk of infection. Because ovulation can result in a high libido, people may be more likely to engage in sexual activities around that time, increasing the risk of infection.
To lower the risk of infection right before your period, Dr. Hlavinka recommends taking a non-hormonal approach and often encourages aggressive doses of probiotics in the days leading up to menstruation.
Watch the video above to hear Dr. Hlavinka discuss when HRT may be beneficial and how IUD may contribute to recurrent UTI.
Probiotics, Biofilms, and Interstitial Cystitis With Dr. Hlavinka
Now that we know a urinary microbiome exists, how can we actively support it?
Within the urinary microbiome, there’s the normal, there’s the quasi-normal and then there’s the abnormal. You can have organisms that are clearly pathogenic and live in the environment and cause no problems whatsoever. Then you can have organisms that are clearly commensal, or considered harmless but in many patients cause severe harm.
Discovering and understanding this is important in treating UTI, especially when we consider how antibiotics may impact the bladder microbiome.
The bottom line is that you do want to not alter that microbiome, and you want to take alternative therapies if you can. You want to get rid of an infection in the easiest way, but when an acute infection does happen, you want to eradicate it because you don’t want to have that become resistant and cause more symptomatic infections.
So when you do get an antibiotic you’re always fighting two battles: alteration in the microbiome and getting rid of the acute infection.
One approach to limiting the impact of antibiotics on the body is to incorporate probiotics. Dr. Hlavinka recommends high quality probiotics with 20 to 60 billion colonies on a daily basis. When probiotics are included in the treatment plan, the immune system becomes enhanced and the body is better equipped to handle the infection.
“What we’re learning is that the gut and its microbiome have tremendous amounts of intelligence and there’s actually a brain gut connection in the microbiome. So the bottom line is being very aggressive with probiotics has been absolutely as essential as my incorporation of next generation sequencing into my therapy.“
– Dr. Tim Hlavinka
How Is Interstitial Cystitis Diagnosed?
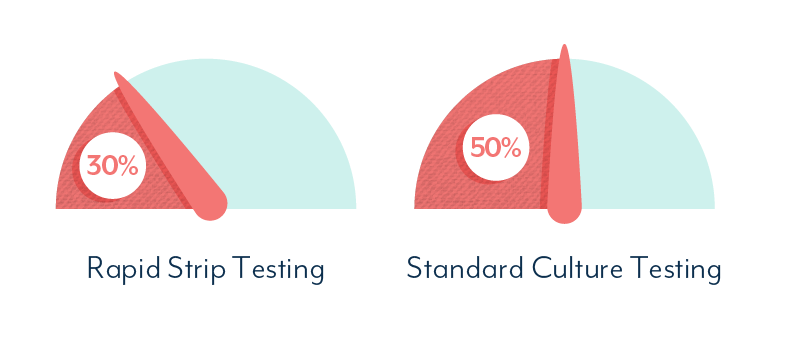
Dr. Hlavinka utilizes PCR and Next-Generation Sequencing frequently as opposed to standard urine culture (SUC). He discovered the limitations of SUC years ago and learned of how they contribute to misdiagnosis. While DNA urine tests also have limitations, the testing is more sensitive and accurate than SUC and can provide better treatment guidance.
Because NGS testing is not without limits, patient symptoms in conjunction with test results are considered prior to treatment. Some physicians may not treat a symptomatic patient because they have a low bacterial load or are only showing organisms that are considered harmless. However, Dr. Hlavinka always takes symptoms into consideration with his patients.
For Dr. Hlavinka, he never assumes an infection is not present unless he has a negative NGS test. For patients with a diagnosis of IC, chronic pelvic pain, pain during intercourse, pain with ejaculation, approximately 55% have shown significant organism loads with symptoms that improve with treatment.
Until a patient’s NGS test is negative, he no longer diagnoses patients with lower urinary tract symptoms with IC.
New Treatments For Interstitial Cystitis, UTI, and Prostatitis?
The approach to interstitial cystitis (IC) in the areas of urology and urogynecology as many thought leaders are beginning to consider that IC could be an undiagnosed infection, according to Dr. Hlavinka. Many patients diagnosed with IC will often use the terminology that they have an acute UTI on top of their IC.
Dr. Hlavinka began recognizing a pattern of IC patients reporting acute infections, but receiving a negative standard urine culture. In these instances, DNA testing became a critical component of his diagnostic procedure.
As an additional step, Dr. Hlavinka has taken biopsies of Hunner’s ulcers in patients with an IC diagnosis. The tissue analyses have revealed infection, and as a result, he is convinced that IC is either bacteria or a bacterial product buried under the surface – similar to that of acne or cellulitis.
When considering the treatment approach for IC, recurrent UTI, and other bladder health conditions, it can be helpful to view the pelvic issues as each a part of a whole constellation. All conditions should be treated alongside one another.
For the recurrent UTI portion of the constellation, Dr. Hlavinka initially uses short courses of antibiotics so he can observe the response to treating specific organisms. Completely eradicating an organism is not always the goal, so the treatment method may be adjusted and testing repeated throughout the process.
UTI And Sex: Should I get My Partner Tested? Dr. Hlavinka Weighs In
Some of the main questions that we get from our audience are around sex and UTIs. We get a lot of questions about how you can avoid UTIs after sex, whether a partner may be contributing to UTIs after sex and many more. Dr. Hlavinka gave us insight into why sex can be a trigger for UTI.
When a symptomatic patient is sexually active, all people involved in the sexual relationship need to be considered, even if they are asymptomatic. In a group of 10 heterosexual, monogomous couples, 6 out of 20 people were asymptomatic. When tested using standard urine culture, only four organisms were reported between all 20 people.
However, when NGS was used, each member of a couple shared the same organism with their partner. This occurred for all 10 couples. Two errors occur when partners are passing organisms between one another: 1. The partner is often not considered. 2. The wrong diagnostic techniques are being used.
As Dr. Hlavinka states, “we need to recognize that there are a whole lot more sexually transmitted infections, and we need to drop the stigma that comes along with sexually related infections.”
Organisms can be transmitted during vaginal, anal, and oral intercourse. In Dr. Hlavinka’s clinical experience, mouth organisms have become more prevalent as people are having more oral sex. The throat and mouth are another area to consider testing between partners.
What are some of the signs to look for in determining if your partner may be contributing to your UTI? For males, the semen may shift from a white, pearly color to having a yellow tint. A change in odor or taste can also be signs that either a male or female partner is exhibiting subtle signs of a microbiome imbalance.
UTI And BV, Yeast Infection And Other Risk Factors
UTI and BV go hand in hand for many people. As do UTI and yeast infection for others. Research has shown that the urinary and vaginal microbiomes are interconnected, so it’s no surprise that organisms in one can have an impact on the other.
One approach to breaking the cycle of UTI, BV, and yeast and preventing future UTI is to consider balancing the vaginal microbiome with anti-inflammatory and pH balanced solutions. At times, vaginal estrogen supplementation may be needed as this cycle of imbalance can create a menopausal state within the vagina.
People are able to come off of antibiotics and break the cycle, but it is typically a more difficult and involved process the longer the imbalances have existed. It’s important to be proactive in these issues and have a plan in place for discontinuing antibiotic treatment.
Pre and probiotics play a big role in Dr. Hlavinka’s approach to helping a patient discontinue antibiotics. Once it is confirmed that bacteria, fungus, and inflammation are not out of control, he strongly recommends patients incorporate oral probiotics and vaginal prebiotic suppositories into their health routine. Rather than waiting for symptoms to return and responding retroactively, patients are better prepared to prevent a relapse of symptoms.
Acknowledgements
Interstitial cystitis, UTI and sex, and the impact of hormones are often discussed topics within our community. While more research is needed in each of these areas, we appreciate the value of clinicians sharing their own clinical experiences. We’d like to thank Dr. Tim Hlavinka for generously sharing his time to answer the questions submitted.
If you’ve found this information helpful, you can support future expert interviews and other projects by contributing to the work that means the most to you. To become more actively involved, become an official Live UTI Free member.
Subscribe to Live UTI Free on YouTube to watch more expert interviews and to be notified when new videos are released.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions in the comments below, or reach out to our team directly.

