Dr Michael Hsieh On Recurrent Urinary Symptoms and Pediatric UTI
As part of our series on recurrent UTI treatment approaches, we spoke with Michael Hsieh MD, PhD.
Dr Michael Hsieh, a urologist who specializes in pediatric urology, is based in Washington, D.C. He has extensive experience in laparoscopic and robotic surgery for urologic conditions, and also runs a bladder biology research group.
Everything you read below is based on our interview with Michael Hsieh. You can also watch our video interview with Dr Hsieh, where we cover many of these topics in detail.
Jump To Section:
- Other Causes Of Urinary Tract Symptoms >>>>
- The link between recurrent UTI and Interstitial Cystitis. >>>>
- Dr Michael Hsieh’s recurrent UTI And Interstitial Cystitis treatment approach. >>>>
- How to make an appointment with Michael Hsieh. >>>>
- How to prepare for a urology appointment. >>>>
- Ask Me Anything with Dr Hsieh >>>>
 | “I believe in personalized medicine for UTI, in the sense that each patient's UTIs are different and each patient is at a different place. Diagnosis, treatment, and prevention should be tailored accordingly, and take into account patient preferences and the pros and cons of various approaches.” |
Other Causes Of Urinary Tract Symptoms
There are many different illnesses and conditions that can cause symptoms similar to a UTI, and it’s important to investigate the root cause.
In our interview with Michael Hsieh, we discussed other potential causes for recurrent UTI symptoms. This list is by no means exhaustive, but will hopefully provide some insight into why seeing a doctor for UTI is a good idea.
Possible causes for urinary symptoms (other than urinary pathogens):
- Endometriosis (of the urinary tract or elsewhere)
- Anatomical abnormality
- Dietary irritants or intolerances
- Drinking too much water (or not enough)
- Pelvic pain syndromes
- Urethral diverticulum (a pocket or pouch that forms along the urethra)
- Urogenital schistosomiasis (a parasitic infection common in some regions)
- Kidney or bladder stones
- Vaginal atrophy associated with Menopause
- Lichen sclerosus
- Hormonal changes associated with Menopause
- Pelvic floor disorder (including organ prolapse)
- Bladder cancer
- Sexually transmitted infection
- Vulvodynia (vulval pain)
- Bacterial vaginosis or vaginal yeast infection
 | “Occasionally patients are just drinking way too much water. And so if I get that sense, sometimes I ask patients to keep a bladder diary where they record their intake and outtake. And then you realize they’re drinking two gallons of water a day, and only weigh 100 pounds. And I point out to them that that’s not typical, and that if they have excessive urine output and urinary symptoms because of that, that’s not so surprising.” |
Because your UTI symptoms may not actually be caused by a UTI, there’s a strong argument for considering seeing a gynecologist, urologist or urogynecologist early on. This is particularly important for patients who have had pelvic surgery or any pelvic injuries or treatment in the past.
Watch this video with Dr Michael Hsieh to learn more about:
- Lichen sclerosus, vaginal atrophy and chronic inflammation
- Menopause, estrogen levels and their link to UTI
- Vestibular vulvodynia, a diagnosis of exclusion believed to be caused by nerve or mast cell overactivation
- Parasites that can trigger urogenital symptoms
Michael Hsieh On Finding The Right Doctor For Recurrent UTI
If you are seeking the help of a urologist, keep in mind that most urologists specialize in male urology, and they are primarily surgeons. In many cases, a urologist may not be helpful for recurrent UTI.
Some urologists, however, have a specific interest in female recurrent and chronic urinary tract infections. It’s important to locate one of these specialists. Please note that Dr Hsieh is currently working with pediatric patients only, and cannot consult with adult patients.
 | “I think unfortunately, some urologists, and I'd like to think it's a minority, get frustrated with recurrent UTI, partly because they feel like they don't have much to offer. They feel even more helpless when the urine cultures are coming out negative. I'm all about patient empowerment, and I encourage patients in that situation to seek out providers who are comfortable managing patients who do get culture negative UTIs, particularly providers who are willing to do enhanced quantitative cultures, or microbiome testing and are open at the very minimum to discussing the literature on non-antibiotic approaches to UTIs." |
The Link Between Recurrent UTI And Interstitial Cystitis
With the rise in the availability of more advanced UTI testing techniques, the possible link between recurrent UTI and Interstitial Cystitis (IC) has once again come under the spotlight.
In the case of IC, where standard urine culture has been unable to pinpoint the cause, DNA sequencing has identified infection in thousands of IC patients.
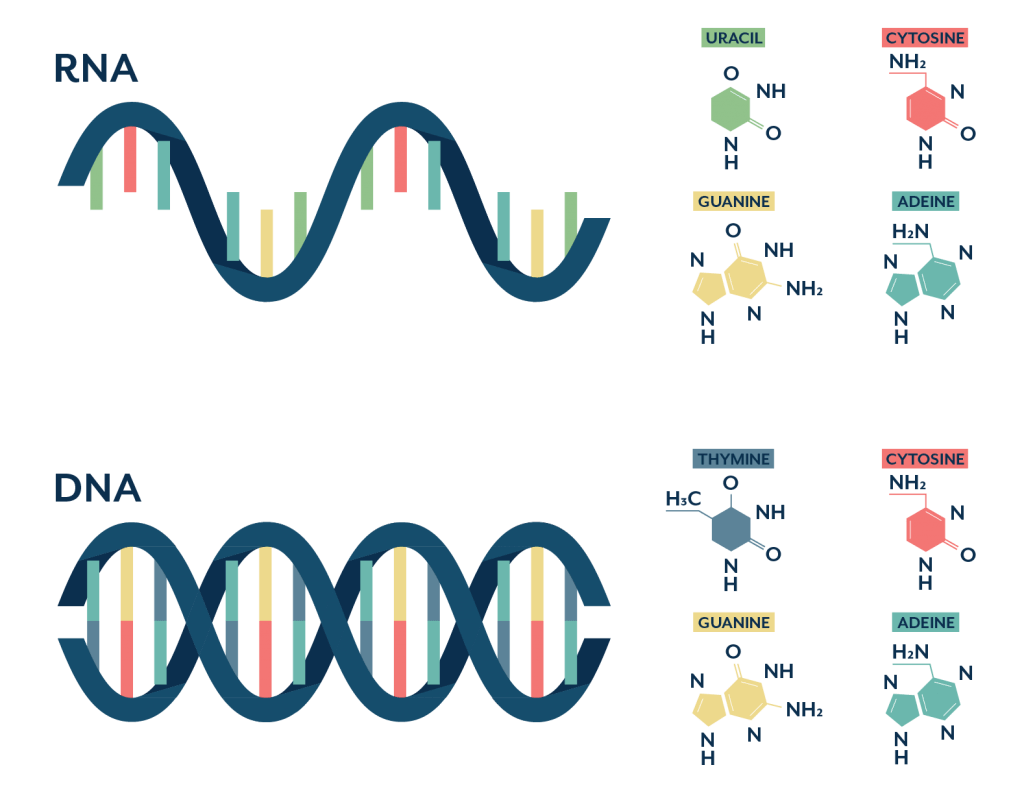
Dr Hsieh uses these testing techniques that look at the urinary microbiome, rather than relying solely on the standard urine culture, which has been shown to be very inaccurate.
 | “I've seen patients who have been labeled as having IC, and in my opinion, they didn't even have sufficient diagnostic interrogation. And on top of that, microbiome analysis clearly shows pathogens in their urine. Then you treat it, and their symptoms go away. So pretty clearly it wasn't any kind of IC in that situation." |
Why Some Urinary Tract Infections Are So Hard To Test For
With persistent bladder infection, UTI symptoms may ebb and flow, or they may be continuously present.
A chronic infection like this is caused by pathogens living within your bladder wall, or in structures called biofilms.
 | In the case of a chronic urinary tract infection, a biofilm is a community of bacterial cells that stick together and adhere to the bladder wall. These cells then produce a protective slime that shields the bacterial community from antibiotics and the natural defences of the body. |
Your body naturally flushes out free-floating pathogens in your urine, but biofilms and pathogens within the bladder wall remain intact…
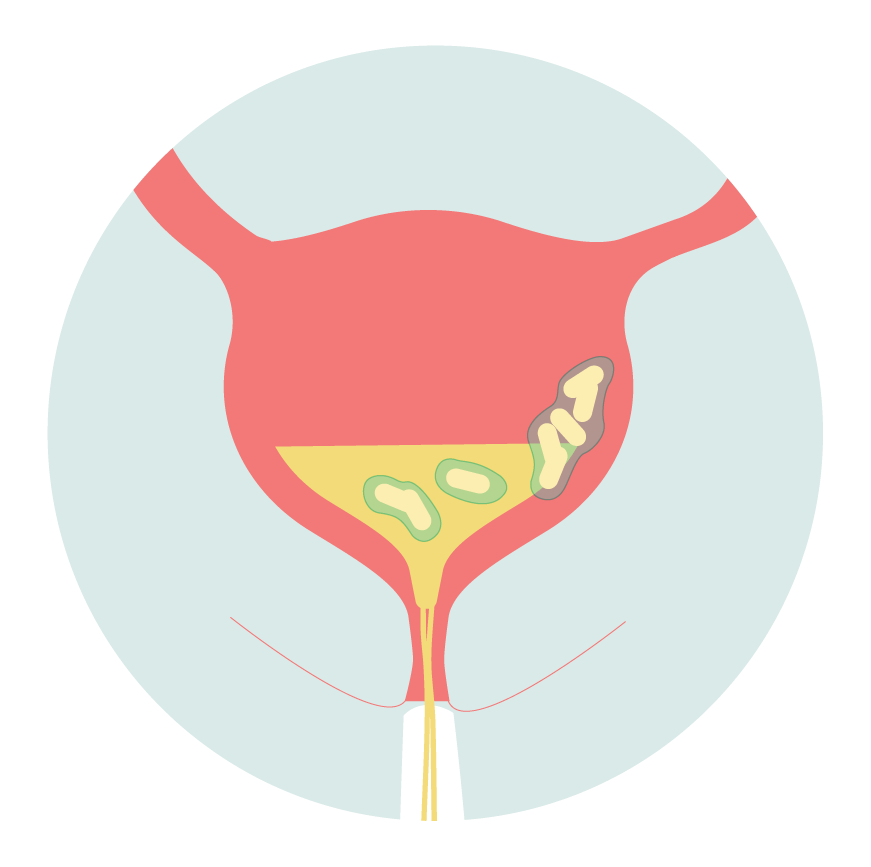
Biofilms and intracellular communities make diagnosis and treatment very difficult as the pathogens contained within them may not pass into your urine, and will therefore not be detected by testing.
 | “I think biofilms play a major role. Although a number of practitioners are reluctant to embrace the concept, in my opinion, it's pretty clear that it's a true phenomenon. It would explain why a given patient can get what seems like an appropriate antibiotic based on antibiotic susceptibility testing from cultured bacteria. Then as soon they stop taking the antibiotic, even if they've taken it for a week or two, the same exact bacterial isolate comes roaring back, with the same antibiotic susceptibility. Why wasn’t it wiped out? Well, I think sometimes it's intracellular bacterial communities, or biofilms." |
Can You Test For Biofilms Or Chronic Infection?
While standard urine culture is unlikely to identify pathogens within epithelial cells, or pieces of biofilms that are shed into the urine, microbiome test methods should be able to.
In this case, you’re not testing to see whether a biofilm is present per se. Instead, genetic sequencing techniques are able to pick up the DNA of bacteria present, regardless of whether or not they would grow on a culture plate.
The limitations of the standard urine culture mean we know very little about what should and should not be in the urinary tract. This also makes it difficult to know what to treat.
Microbiome testing is helping scientists find organisms in the urinary tract that were never considered possible. For recurrent UTI sufferers who receive negative urine culture results, this newer type of testing could provide answers.
 | “With Microbiome testing, you don't often get one bacteria. Certainly, I have found the usual suspects like E. coli. I’ve even detected some STIs, and anaerobes that can’t be grown by culture. Sometimes, you get long lists of bacteria that we know very little about, and I'll do extensive literature searches and sometimes barely come up with one or two papers. And so what I generally do in that situation is to try and figure out which are likely to be pathogenic, and treat those. This is a really different way of prescribing antibiotics compared to when I was trained." |
Dr Hsieh’s Recurrent UTI And Interstitial Cystitis Treatment Approach
The key to Michael Hsieh’s approach to recurrent UTI treatment is to evaluate each patient’s case individually. He also makes a point not to dismiss patient symptoms. In Dr Hsieh’s own words:
“UTIs are caused by interactions between our bodies and bacteria that are perceived as harmful by our immune system. How these interactions play out are different not only for every person, but also every infection. We are all unique genetically, including genes that determine how our immune systems react to infections, and properties like how “sticky” the lining of our urinary tracts are for bacteria.
These genes are subject to changing their activity by epigenetic alterations, which are reversible ‘marks’ that our bodies place on DNA in response to environmental factors, such as stress and prior infection exposures.
Layered on top of all of this is our microbiome, the community of thousands of bacteria living in and on our bodies, including in the urinary tract. Bacterial members of the microbiome can differ significantly from one another, even when of the same species. Thus, how these highly unique bacterial strains interact with our epigenetically modified genes can result in very different UTI symptoms and patterns for each patient.”
There are two main differences between the approach of Dr Michael Hsieh, and the approaches of many other practitioners. First, is testing.
Michael Hsieh uses microbiome analysis to supplement testing of patients, especially if they have culture negative infections. He also uses Expanded Quantitative Urine Culture (EQUC), which has been shown to be much more accurate than a standard urine culture.
Second, there is a difference in Dr Hsieh’s therapeutic approach. While antibiotics are still a mainstay for treatment and prevention, he also tends to recommend non-antibiotic alternatives that have reasonable data in favor of them. These include certain probiotics and certain cranberry products.
How Long Does Recurrent UTI Treatment Take?
Occasionally, Dr Hsieh sees his patients turn around very quickly. Some patients who have had multiple UTI episodes in a three to six month period, have changed their regimen and quickly become symptom free.
Unfortunately, this is not typical. Most patients require six months or longer of management, before a resolution of their symptoms. Dr Hsieh reports that around 80% of his recurrent UTI patients do recover completely.
The standard form of treatment for UTIs is antibiotics. Antibiotic resistance is becoming more prevalent in the UTI community, but there are other circumstances in which UTI patients do not respond to antibiotics.
Theories as to why UTI symptoms are sometimes not alleviated by antibiotics:
1. A biofilm has developed in the bladder, in which the bacteria might not only successfully gain protection from the immune system but also from antibiotics.
2. E. coli reseeds in the patient’s gut and spreads to the urinary tract.
3. There is also the discussion of whether this bloom of E. coli in the gut could be followed by communication between organs and bacteria, leading bacteria already present in the urinary tract to multiply upon their realization that the body’s immune system is compromised.
Dr Hsieh expands on these theories in Part 2 of our video interview.
Bladder Instillations For Recurrent UTI Treatment
Dr Michael Hsieh typically starts patients on an oral antibiotic, along with probiotics and other supplements. If this approach does not prevent breakthrough symptoms, bladder instillations may be the next step.
Bladder instillations enable the delivery of high concentration antibiotics directly to the bladder, via a very small, pre-lubricated pediatric catheter.
Of course, this method is technically more invasive, requiring the insertion of a catheter through the urethra, but it’s likely it reduces any impact of antibiotics on the gut.
For recurrent UTI patients who have taken numerous rounds of antibiotics, this can be an important consideration.
Patients are trained to administer bladder instillations themselves, usually once or twice per day for various periods of time. The ideal treatment regimen for bladder instillations is still unknown.
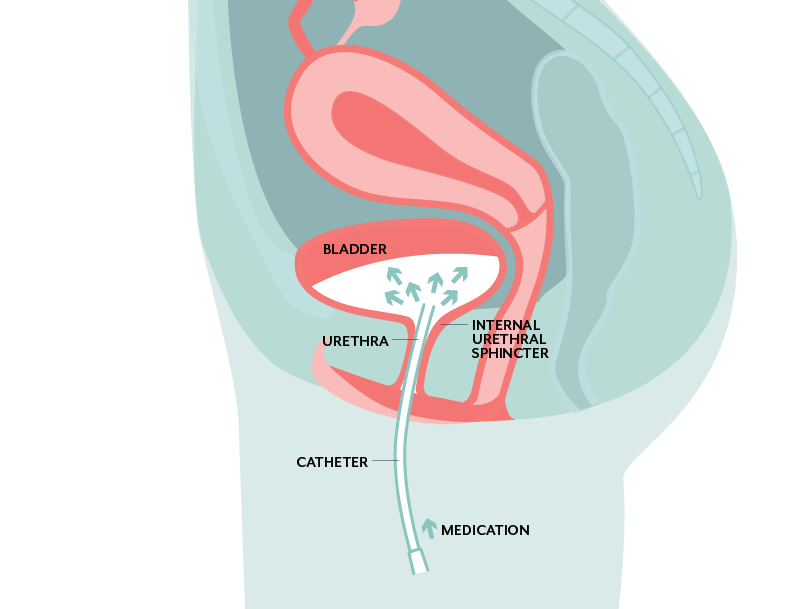
The antibiotic is placed into the catheter, which is then inserted through the urethra. The medication is delivered into the bladder, and ‘held in’ for as long as possible, before it is passed as urine normally would.
Dr Hsieh often recommends delivering the instillation right before bed time, to maximize the time the antibiotics are in the bladder.
Of the patients treated with bladder instillations, Dr Hsieh has seen good responses in many. The response is not necessarily immediate, but this approach does appear to be a good option for certain patient populations.
Is Antibiotic Treatment Necessary For UTI?
It was long thought that urine is sterile. This mistaken belief is based on old studies that relied upon the ability to grow bacteria in the laboratory.
These studies failed to grow bacteria out of the urine of most healthy individuals, and this led scientists to believe that the urine is typically sterile.
However, the advent of molecular, non-culture-based methods to detect the bacteria in and on our bodies (the microbiome), has revealed that the urine may never be sterile, even in healthy people.
 | “Even as a physician who has conducted microbiome research for a number of years, I was initially skeptical of urine microbiome testing as a means to diagnose UTI. However, I have had multiple patients who had standard urine cultures that lined up exactly with their microbiome testing, and quite a few patients who had “positive” microbiome testing followed by a subsequent UTI. This strongly suggests that microbiome testing is not only accurate in the right setting, but also may predict imminent UTI in some patients." |
There are certain ramifications of the discovery of the urinary microbiome. One is that asymptomatic bacteriuria should not necessarily be treated.
If there is supposed to be bacteria in the urinary tract, why would we try to wipe them out when the patient is not experiencing symptoms?
A caveat to this is UTI during pregnancy. It does appear that treatment of asymptomatic bacteriuria may still be important in this patient population.
A second consideration raised by the discovery of the urinary microbiome, is how the use of any antibiotic may impact the balance of bacteria in the urinary tract. It can no longer be assumed that antibiotics do not cause issues in the urinary tract, as much as they may also treat or prevent them.
For these reasons, Dr Hsieh may recommend a non-antibiotic therapy approach, particularly in patients who have had adverse experiences with antibiotics, or who experience very mild UTI symptoms.
How To Make An Appointment With Dr Michael Hsieh
Dr Hsieh currently sees pediatric chronic UTI patients at the Children’s National Health System. You can visit the link for more Information on how to make an appointment.
Appointments with Dr Hsieh are covered by healthcare insurance in most cases. For uninsured patients, Dr Hsieh does his best to make fees reasonable and within their financial means.
What Types Of Patients Can Make An Appointment?
Dr Hsieh’s office is open to all pediatric patients. This includes female and male teenagers and children of any age, including fetuses.
Many of Dr Hsieh’s patients have more complex anatomy due to prior surgery or congenital urologic conditions, however, a significant number of patients are sufferers of recurrent UTI who are otherwise healthy.
UTI In Children And Adolescents
For children and adolescents with recurrent UTI, it’s important to see a pediatric specialist that can help.
Dr Hsieh’s specialty in pediatric urology extends to transitional urology for adolescents. What is transitional urology?
Patients born with congenital genitourinary conditions require complex care early in life, but also as they progress through adulthood.
Transitional urology provides continuity in this care, supporting these patients through childhood, adolescence and adulthood.
 | “So the best analogy is: kids with congenital heart disease rarely used to make it through childhood, even with the best attempts at care. But both medical and surgical care have improved. Now these patients routinely survive to adulthood. As a result of that, then there was a new adult patient population with congenital heart disease that required adult congenital cardiologists or basically transitional cardiology. The same thing has happened in urology, there are a number of congenital urologic diagnoses that used to routinely, unfortunately, lead to death in childhood. But now almost all these patients survive to adulthood. That's given rise to the field of transitional urology." |
As a result of Dr Hsieh’s specialty in pediatric urology, he sees many young patients who experience recurrent UTI and have an otherwise healthy urinary tract.
Dr Hsieh continues the discussion around age-related behaviors in preventing and treating UTIs in our updated video interview.
How To Prepare For A Urology Appointment With Dr Hsieh
The more information you can provide regarding your own experience with UTI, the better. Dr Hsieh recommends you prepare as much of the following as you can:
- A timeline of your UTI symptoms – when they started, how often you experience them, are your symptoms worse at particular times?
- A timeline of when you have started and stopped antibiotics, and which antibiotics you’ve taken when, if you know
- All your previous urine culture test results, along with any associated urinalyses, and antibiotic susceptibilities
- Any test results from other types of UTI testing you have done
- Reports plus original imaging from any type of urinary tract imaging you have completed, including ultrasounds, DMSA scans, MAG-3 Lasix renal scans, MRI, CT, retrograde pyelograms.
This may seem like a lot, but it’s important for urologists to look at all patient results and imaging. There could be subtleties relevant to UTI that the person who prepared the results may not have commented on.
If you have completed any recent testing and have not received your results before you attend your appointment, it’s important that you grant Dr Hsieh access to the results, prior to your appointment.
 | “After five years of experiencing recurrent UTI’s and being on antibiotics, finally for the past seven months I have been symptom free of UTIs and most urine tests showed no bacteria. I think that the supplements Doctor Hsieh recommended have helped. In addition, Dr. Hsieh suggested I have a microbiome testing of the urine. The results of this test showed that I had biofilm/intracellular bacterial communities. Which allowed him to treat me accordingly. I could not believe that I was symptom free and felt normal for the first time in many years!” Maria, Patient |
Ask Me Anything With Dr Hsieh
We recently collected questions for Dr Hsieh from our community, and you can find his answers below.
Question: Can parasites infect the bladder?
Dr. Hsieh’s Response:
The only parasite which infects the human bladder is the Schistosoma haematobium worm. This parasite is only found in certain parts of the Middle East and sub-Saharan Africa, and infection occurs through exposure to infested water. There is no sexual transmission of this parasite. Symptoms of urogenital schistosomiasis (infection with S. haematobium) include hematuria (blood in the urine), and a range of urinary symptoms, such as frequency, urgency, and pain with urination.
Question: With DNA-based testing methods, how do we know if the bacteria are alive or dead?
Dr. Hsieh’s Response:
It is important to know if bacterial DNA being detected is from live bacteria, since only live bacteria would cause a UTI. This has been one of the major criticisms of current commercially available bacterial DNA tests.
Newer methods that selectively detect DNA from live bacteria are currently under development. We have developed such a method, and have also shown that in mice with antibiotic-treated UTI and negative post-antibiotic urine cultures, many still have DNA from live bacteria detectable in their urine.
This suggests that perhaps some patients with persistent, post-antibiotic UTI symptoms and negative urine cultures may have residual bacteria.
Question: Is it possible to diagnose an embedded UTI?
Dr. Hsieh’s Response:
The concept that UTI can persist or recur is accepted by patients and providers. Recurrent and persistent UTI remain a clinical diagnosis, based on patient symptoms and testing results.
Although a bladder biopsy has been used in a research setting to confirm that there can be depots of bacteria within the lining of the bladder, routine bladder biopsy for patients with suspected UTI carries risks of bleeding, infection, and perforation of the bladder.
At this stage, diagnosis continues to be based on patient symptoms and clinician experience.
Question: In what circumstances do you recommend bladder fulguration?
Dr. Hsieh’s Response:
Bladder fulguration is only appropriate for patients with specific inflammatory lesions in their bladders, such as trigonitis and other forms of chronic infection.
Office cystoscopy to look in the bladder to identify these lesions is an option, but fulguration itself requires anesthesia because it is painful. Some providers offer cystoscopy under anesthesia as a first option so that any lesions seen can be immediately fulgurated.
Question: Can UTIs cause confusion, delirium, insomnia and irritation?
Dr. Hsieh’s Response:
Symptoms caused by UTI can be quite different between younger versus older adults. Mental status changes, such as confusion, delirium, insomnia, and irritability can be more common in older adults.
In addition, older adults tend to have fewer “classic” UTI symptoms, such as urinary urgency and frequency. This can make diagnosing UTI challenging in older adults.
When older adults have mental status changes, it is worth considering the possibility that it is being caused by a UTI.
It is unclear whether UTI in older adults only causes delirium, which is temporary, or if it can also precipitate dementia, which is permanent.
Question: Why can you be fine one day on long term antibiotics and awful the next day?
Dr. Hsieh’s Response:
It is unclear why UTI symptoms can fluctuate while patients are on antibiotics. There are several theories as to why UTI symptoms can fluctuate in some patients while they are taking antibiotics. Sometimes patients refer to this as a ‘flare’.
One theory is that bladder “injury” caused by a recent UTI can cause symptoms very similar to that of an ongoing UTI, and that these symptoms fluctuate until the bladder heals.
Another theory (which does not exclude the first theory) is that antibiotics may eliminate bacteria floating in the urine or on the surface of the bladder lining, but then bacteria inside the bladder lining may re-emerge and lead to recurrent symptoms.
Question: For UTIs only related to sex, should my partner get tested?
Dr. Hsieh’s Response:
UTI are likely triggered by sexual activity due to mechanical factors (pushing of bacteria up the female urethra and into the bladder).
Although UTI are not traditionally considered sexually transmitted infections, there is some evidence that potential UTI-causing bacteria can be passed between sexual partners, even if the transmitting partner is asymptomatic.
However, it is not clear that any such bacteria transmitted in this fashion result in UTI caused by those bacteria.
Question: What do you think of phage therapy for antibiotic resistant embedded UTI?
Dr. Hsieh’s Response:
Phage therapy for UTI is promising. Phage are viruses which infect bacteria. There is promising research suggesting that “cocktails” of phage could be used to treat UTI without having to resort to antibiotics.
One challenge that this approach would need to overcome includes quickly and reliably making tailored phage mixtures for individual patients, since phage are highly specific for bacterial species.
This means that each type of phage usually only targets a single bacterial species and sometimes just a strain within a species. So the bacterial species believed to be causing the UTI must be identified in order to ensure the right phages are used.
Another important question relevant to use of phage for UTI is whether phage would be able to eliminate bacteria that have gone into the cells lining the bladder.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. And as always, if you have any questions or comments, you’re welcome to leave them below.

I’ve been on 7different antibiotics for a year now for UTI’s. Nothing is helping but I believe I have vaginal atrophy. Seems pure aloe gel relieves the burning. Does VA also cause lower back pain? I also have spinal stenosis. Doctors can’t seem to find out what’s going on.
Hi Christine, Urogenital symptoms can cause pain in other places. It’s best to speak to a clinician as we aren’t medical professionals. If you have any questions or would like clinician information, please feel free to get in touch. Best wishes, Issy
Does Dr Hsieh accept adult patients as of 2023? I contacted on of the departments he is listed in, and they told me he only accepted pediatric patients. Could you please clarify on that? Thank you
Hi Maria, I have sent you an email. Let me know if there is anything I can help you with, Molly.
Hi, I was wondering if it was at all possible to book an appointment with Dr. Hsieh as a non-American? The doctors where I’m from are dismissive and not very good, is it at all possible to get a treatment plan with him?
Author
Hi Izzy, as mentioned in the article, Dr. Hsieh is no longer able to work with adult patients. He is able to book pediatric appointments only. Melissa
(cont.) I have had to travel to DC a few times but Dr. Hsieh has also been willing to mantain constant communication with me over email. Luckily my insurance has covered all my visits and treatment. If you feel like you are at the end of your rope, like I was when I first went to see him (at some point I was even unable to work because my symptoms were so bad) I highly recommend that you don’t give up and explore new options.
Author
Hi Andreina, thanks for sharing an update! I’m so glad to hear you feel you’re on the road to recovery. That’s such good news :). Melissa
(cont.) I have lived in New York since 2010, and I believe this move and the stress involved in embarking on a PhD, plus a particular sexual partner and perhaps not appropriate early treatment, had something to do with my condition becoming chronic. I have tried EVERYTHING and seen many urologists in New York but none was close to helping me as much as Dr. Hsieh has, and for that i’m so very grateful (to him and this blog).
I keep having uti and it’s really bugging me
Author
Hi Nichole, you are welcome to get in touch with us directly if you have any questions. It helps to know where you’re based. Melissa
I have seeing Dr. Hsieh since Oct 2019, I found him through this website. I am happy to report that I am on the road to recovery thanks to his approach. I still have to wait a bit until I can say I am UTI free but after a second surgical procedure to cure lessions in my bladder (oct 28 2020) I have felt much improvement. I have suffered what I believe has been a chronic UTI since 2012, with positive cultures for antibiotic resistant e.coli and sometimes klesbisella.
I self Cath due to Over stretch bladder Since then I have had 9 infections in 14 months Recent I have had Relapse UTI from e coli I believe I To be caused by intracellular Biofilm infection. IsThere any treatment for this I am 65 year-old woman who before this never had a UTI I am suffering and very discouraged
Author
Hi Marianne, we hear many similar stories. Can you send me an email and let me know where you’re based so I can share relevant information? Melissa
I leave in Sacramento California
Hi Marianne, I’ve sent through some info via email. Susy
Can I book an appointment with the doctor?
Author
Hi Sneha, you can use the information in the article above to get in touch with Dr Hsieh. As it mentions, Dr Hsieh currently sees chronic UTI patients at both the Children’s National Health System, and George Washington University (GWU) locations. I hope that helps. Melissa
I have been suffering with chronic uti for over 40 yeats. Every so often I need to take anti
biotics but I always have pressure and pain as well as urges to go frequently to the bathroom.
I tried acupunture it helped a bit and I would like to know with what other means I can alleviate the problem.
Best regards,
Author
Hi Rizi, I’ve sent you a few emails over the past months but I’m not sure you’ve received them. Can you send me a direct message to let me know? Melissa