Probiotics And UTI, Biofilms, And The Urinary Microbiome
We know that probiotics and UTIs are a hot topic, so we wanted to interview an expert to help us break it down.
Taking his clinical experience into account, Dr. Tim Hlavinka discusses the connection between the gut, vaginal and urinary microbiomes, and how probiotics influence each area.
During our interview, Dr. Hlavinka also gave us insight into his experience with biofilms and evidence of their presence in Hunner’s ulcers.
To learn more, watch the video or read the full transcript below.
Jump To Section:
- Video 2 Transcript: Probiotics And UTI, Biofilms, And The Urinary Microbiome >>>>
- Oral Probiotics and UTI >>>>
- Antibiotics for UTI and the Urinary Microbiome >>>>
- Vaginal Health Influence – Probiotics and UTIs? >>>>
- IC or UTI? How Biofilm may be Involved >>>>
- Hunner’s Ulcers and Biofilm Communities >>>>
Video 2 Transcript: Probiotics And UTI, Biofilms, And The Urinary Microbiome
Melissa: So let’s move on to a discussion more about the urinary microbiome and the yeast or BV connection with recurrent UTI. Maybe you can explain a little bit more about the urinary microbiome. Now that we know that it exists is there a way that we can actively support that?
Dr. Hlavinka: We do know now that there is a urinary microbiome and there’s the normal, there’s the quasi-normal and then there’s the abnormal. And you can have organisms that are clearly pathogenic and live in the environment and cause no problems whatsoever. Then you can have organisms that are clearly commensal, or harmless quote unquote and in many patients cause severe harm, in a given patient who may be susceptible to that microbe.
By and by there are rules but I have found that with patients and next generation sequencing and identification and treatment that I didn’t get to make the rules, they do. And what I thought were the rules from what I learned in microbiology and infectious disease therapy and pharmacology were wrong because it just doesn’t work that way.
I think that we have to be adaptive as providers to these lessons, just like the microbes are adaptive in keeping in our bodies and causing havoc. So that’s the problem. We’re dealing with some very, very ancient organisms that have a real keen survival mechanism and they’re tough to get rid of.
So discovering that first is the most important thing and absolutely the next question is ‘do antibiotics impact the bladder microbiome?’ I don’t need to tell this group the cascade of events that happens with their first UTI treatment. I hear these stories that end up being two or three years long after that for the patient.
So the bottom line is that you do want to not alter that microbiome, you do want to take alternative therapies if you can. You do want to get rid of an infection in the easiest way. But when it does happen you want to eradicate it because you don’t want to have that become resistant and you don’t want to have it cause more symptomatic infections.
So when you do get an antibiotic you’re always fighting two battles, alteration in the microbiome and getting rid of the acute infection. There’s like two swords I have to have and I’m not very good at fencing anyway.
So the bottom line is, it’s the scourge of my existence when that doesn’t work. When it works I get to be the hero and pat myself on both shoulders, but when it doesn’t then the patient and I have to sit there with a chagrined look on both of our faces and decide what to do next.
Oral Probiotics and UTI
Melissa: So in terms of the urinary microbiome, is it linked to the vaginal microbiome? And then the question again is, can probiotics help in either location?
Dr. Hlavinka: So if we’re going to get into probiotics, I mentioned them before. I’m a firm believer in probiotics. I was very fortunate to meet a provider about 20 years ago who was a GI doc who was treating C. difficile overgrowth and symptomatic C. difficile, which is clustering difficile and a really terrible antibiotic complication that causes severe diarrhea and can even cause bleeding and death in the worst case.
And many people have fear of that and for a lot of providers the fear of creating C. difficile is the reason why they don’t treat any infections aggressively and they won’t tell you that, but I will tell you that.
I’m not afraid of it. I’m not afraid of that because I got aggressive with probiotics. What you buy over the counter typically, or the doctors recommend is not at all adequate. You need on a daily basis we need between 20 and 60 billion colonies of microbes in our gut – new ones. And it’s very difficult to get that with diet.
Now, if you have enhanced kimchi and things like that where somebody’s actually fermenting and creating a product, a natural product, that does have it, but even then you don’t know what you’re getting and you don’t know what organisms.
A good quality natural probiotic with 10 organisms and at least 20 billion per capsule that is shelf-stable so you don’t have to worry about refrigerating it. Enteric coated so your stomach acid doesn’t chew it up. That’s the other thing, if you drink these liquids your stomach acid chews it up, and you certainly don’t take it within an hour or two of taking an antibiotic because the antibiotic will kill it all.
So a lot of really simple practical things about probiotic use, we don’t do. And I will tell you, the infectious disease doctors just wagged their finger at me and told me what I was going to experience when I did Microgen and all the next generation sequencing treatments and multiple antibiotics. I have not had a single case, knock on wood, of C. difficile. In fact I don’t even think I’ve had any antibiotic related complications, all right.
And that is absolutely rare and it’s because my patients know when they come to me for recurrent UTIs, part of the prescription is not just here’s your antibiotic, take it and come see me in two weeks, let’s check another culture. It’s, here’s the program for getting rid of your infections, and getting on probiotics yesterday is going to be the most important thing.
And so how does it alter it? Well you create, as I said, that fight between normal and abnormal microbiome and you what you do is you tilt the scales more toward the normal microbiome which enhances the immune system.
What we’re learning is that the gut and its microbiome have tremendous amounts of intelligence and there’s actually a brain gut connection in the microbiome. So the bottom line is being very aggressive with probiotics has been absolutely as essential as my incorporation of next generation sequencing into my therapy. And keeping that healthy and its impact on the immune system has a profound effect on my impact on patients with infections.
Suppository Probiotics and UTI Treatment
Melissa: Do you also recommend suppository probiotics?
Dr. Hlavinka: I’d say that that is different. If we can do it by oral probiotics, I prefer that because it’s much easier and simpler. It’s sometimes hard to get it right and I’ve actually made things worse.
I tend to want to stay away from the vagina when there’s antibiotics because I’ve seen these circumstances where this and that chemical compound and refresh and replenish and natural this and that and and then all of a sudden who knows what the chemical environment is like in the vagina.
Restoring a homeostatic level and normal vaginal chemical and microbial environment to me is the most important thing to prevent the next infection. And so many times what we’re doing is just kicking the can down the road or disturbing that further and I prefer to stay away and do simple things. But yes I have used all of those, I’ve used all of those when necessary.
Long-Term Antibiotics for UTI and the Urinary Microbiome
Melissa: Do you think long-term antibiotic use actually destroys the bladder microbiome entirely, and can you ever overcome that if you have been down that road?
Dr. Hlavinka: That’s a very good question. That’s controversial. At best I would say that it depends on the pace and severity of infections. If a patient is getting very frequent, very severe infections I have to kind of take that gulp and take a chance on doing that with long-term antibiotics knowing that that tilts the risk benefit more toward benefit.
If she’s the kind of patient who comes in and every time she gets antibiotics it costs her six months of yeast infections and BV and vaginal alterations then I say no, let’s not change that anymore, let’s try to restore it.
I’m not to the point of where the GI doctors are, of giving microbes in the gut to restore that but I would say that that’s a possibility we might be doing in the future in the bladder for people if we could find the right mix.
You know what their normal microbiome was before say, measure it, treat them see how that’s altered and replace anything that might be a beneficial organism.
Melissa: How far away do you think we are from that kind of technology?
Dr. Hlavinka: With next generation sequencing I wouldn’t be surprised if it’s not too far because they are already giving fecal transplants in GI these days and that’s as successful as anything for C. difficile and a lot of the irritable bowel and all of that.
So we’re just behind that. That is going to be for even me, a very aggressive urologist with urinary tract infections, that’s going to be hard for me to accept is putting bacteria in the bladder that I always wanted to be sterile.
Can Vaginal Health and Probiotics Influence UTIs?
Melissa: So you briefly mentioned yeast and BV. I was hoping you could explain the difference between AV and BV and how you go about testing for either?
Dr. Hlavinka: So you’re talking atrophic vaginitis right, and bacterial vaginosis right? So atrophic vaginitis can – any kind of vaginitis, of course vaginitis is a generic term for inflammation of the vagina and it can come from many causes.
It can actually be chemical if you have say, for instance if you’re putting metronidazole suppositories in the vagina and to treat BV, you can get a chemical vaginitis. I’ve seen that happen where the patient for all intents and purposes had a chemical burn in the vagina from the multiple metronidazole suppositories being put in there to treat the BV. And when we stopped them magically the vaginitis went away.
But again, the ability to detect the right organism is so important and you cannot tell. I can have a 28 year old that’s been on the pill for 12 years and I can’t tell if it’s BV or atrophic vaginitis because she probably is estrogen deficient and the problem is that the PCR machines (and that’s called polymerase chain reaction).
And let’s just take a minute to at least say the difference between PCR and next generation sequencing – they are different detection mechanisms and I’d like to wait until we get to the section on testing to go further into how PCR looks for a given set of organisms. It’s a preset test.
In other words, if there’s 28 organisms in the urinary panel for instance, and you got organism number 29 or 30 it’s going to say negative, I don’t find anything all right. So that is part of the problem with BV and atrophic vaginitis and I keep trying to tell my gynecology colleagues, if you’re not doing NGS you don’t know what you’re missing and you’re treating these people incorrectly.
And lo and behold, well I get them all. They come into my office and I’m seeing and I’m identifying them and making them happy. Because we are seeing a ton of resistant BV and we’re seeing a lot of atrophic vaginitis and younger women that need estrogen therapy.
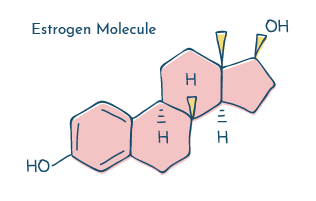
And maybe that’s all they need because younger women will respond more quickly to the estrogen therapy. So that I hope answers that question on how important it is to distinguish between the type of vaginitis – that it is.
Vaginal Infections and UTIs – The Connection
Melissa: Really important. And going back to again the yeast BV connection. A lot of people say they think that yeast infections or BV are actually causing the UTIs. Is it possible that this kind of imbalance is the reason that they’re experiencing urinary symptoms?
Dr. Hlavinka: Absolutely. Any alteration in the vagina, like I said, putting that metronidazole suppository in there, treating with an antibiotic, treating the BV, treating the yeast infection – you are changing the very complex microenvironment of the vagina.
And any alteration of that, you can change the vaginal pH one point and it absolutely completely changes the urinary microbiome. You can change the exudate, the vaginal exudate by chemical change you can irritate the vaginal wall causing edema or swelling of the vaginal epithelial cells, such that they become more fragile and susceptible to ulceration during intercourse and invasion by bacteria.
So all of these things are very exquisitely intertwined in terms of maintaining proper vaginal health and prevention of any infection, be it urinary tract or vaginal.
UTIs and Sex – Transfer of Vaginal Organisms
Melissa: You just mentioned sex as part of the potential issue here. Is it possible that during sex you can transfer organisms from the vagina to the urinary tract and that’s where the problem is coming from?
Dr. Hlavinka: So when we are in our training we hear about a classic study done in the 50s that took a hundred women and they catheterized them before and after immediately after intercourse.
98 of them had bacteria in the bladder and again this was not a culture this was just a detection, but it was a highly centrifuged ultracentrifuge specimen. So they were looking. So almost every woman gets microorganisms in her bladder during intercourse, it is just the mechanical aspect of inner vaginal intercourse.
And that of course will happen with any sort of insertional devices. And I don’t want to get into oral sex versus vaginal penetrative sex but there still are microorganisms there too. But the bottom line is, that happens. So what happens? You’ve got a healthy system, not an aggressive organism, you void it out no problem.
Well the issue is, is that intercourse can create more risk for infection because of that. So every woman gets them in there. So under the circumstances of the vaginal microbiome and risk for infection and urinary microbiome – absolutely you’re going to – whatever’s in the vagina is going to get in the bladder.
And what we have to do make sure that it doesn’t set up shop. And that is the void before and after. The simple things like that. Avoid positions that may be causing you problems. You know perhaps if some people need to shower, and I believe – are we going to get into the issue of passing an infection between partners in the next section?
Melissa: Definitely, in a different section yes.
Dr. Hlavinka: So that certainly is something to identify. And most of the time showering does help – that won’t eradicate it but most of the time showering before intercourse if that you’re susceptible.
Melissa: And do condoms help at all with the transference?
Dr. Hlavinka: So, unfortunately it is a mechanical aspect of intercourse that causes this vaginal microbiome to get into the bladder. Now if a man has an infection say for instance he has a prostatitis or chronic urinary tract infection the condom might help prevent that and again we can explain that more in the section about couples passing infections back and forth.
IC or UTI? Evidence of Biofilm Communities in Bladders
Melissa: Okay, sure. So while we’re still talking about the urinary microbiome I wanted to ask a few questions about biofilms as we received some from our audience. The first is, what is your understanding of the involvement of biofilms in recurrent UTI?
Dr. Hlavinka: We really didn’t understand that environment at all and in urology we thought that microbiomes were other specialties’ problems, like orthopedics, wound care, people who did implants. Those of us that did urinary tract implants knew about microbiomes and biofilms. But the bottom line is that we didn’t really think that that applied to the bladder.
Now maybe in people with kidney damage who had sort of stagnant areas in the kidney and they sloughed these parts of the kidney and there was kind of a chronic kidney infection, yes we thought that would be the case but we couldn’t identify them. All we could do is get a urine that they voided out and sent that for a culture, and we missed so much.
So the capacity to detect an infection, its location, is undergoing revolution not just in urology but across the spectrum of organ systems. So for instance I just heard about a doc, a urologist in Loyola of Chicago who is studying actual different parts of the prostate and the different microbiome in different parts of the prostate.
I have no doubt that that will happen with the bladder also. The bottom line is that I’ve long suspected the persistence of a biofilm in the urinary tract as the cause of a persistent infection. And the reason is that we used to see this thing we call trigonitis.
Trigonitis was this area of the bladder where the ureters come in just inside the bladder from the urethra and it was sort of this filmy layer, whitish layer. Well we thought that was just a plaque in menopausal women that was due to lack of estrogen. Well, that was because we’re dumb old male urologists and really didn’t care because we were going to burn it or biopsy it or something by gosh, or do a urethral dilation, we’ll see you later honey. And that always bothered me.
Also I used to see what we called cystitis cystica. Basically it’s acne of the bladder. You’ll see these little tiny pimples in the bladder and they’re pustules. Okay what does pustule mean? Well pustule means full of pus and pus is an inflammatory liquid. So just like if you pop a pimple, well that’s got bacteria, it’s got propionibacteria and acnes and all that other stuff. There’s infection and white cells and all that other stuff.
Well, that I’m convinced is in the bladder. I also saw patients who had no IC symptoms have these florid ulcerations and cysts and and plaques formed throughout the bladder and you know, should I have biopsied them back then and taken a piece of it to look for microbes? I should have but then we didn’t have any means of detecting them so that would have been overly invasive.
Now I’m doing a lot more of that. I’m going in and sampling these areas. I’m sampling the normal bladder. I’m sampling these ulcers, these plaques. We’re finding that these are full of bacteria. They’re full of inflammatory response and no doubt that they are a component of the persistent infection conundrum that we’re facing.
Biofilm Communities Observed in Hunner’s Ulcers Resections
Melissa: That’s very interesting because you do often hear that one of the signs of IC is these Hunner’s lesions and that that is an indication you have IC and therefore have to manage this disease forever, though I have spoken to other clinicians who say it’s a sign of infection potentially and that it may be able to be treated. So if you see these lesions, you do a biopsy, find microbes, do you then initiate treatment as you would for another kind of UTI?
Dr. Hlavinka: Well to start off I’m glad we’re going into that right now because it segways into discussing this and as a parenthesis please ask those providers to contact me.
I’ve done three IC patients now with their Hunner’s ulcers and I resect them. Now, you’re supposed to resect the Hunner’s ulcers but I thought that didn’t make sense, it’s just going to cut out an infection or you know cut out a scar or an ulcer but that is effective cut them out.
But what I did was, in these three patients, and the patients agreed to it – again this is no clinical trial, they don’t have an institutional review board – but they were miserable. And once I got next generation sequencing I felt that there was a capacity to give them an answer.
So before resecting them I biopsied them and I found a biofilm with multiple organisms. I treated them. In two of them it went away and the third one it did not and I had to resect it, but she’s better after that and we found that there was a different organism in an area that I hadn’t biopsied. So I’m going to resect all of them now and send them because I feel like that’s going to leave potential infection behind.
It’s a short early series but this is my process now and I discuss this with the patients and I believe that more and more IC experts should be getting on board for this. Again, they don’t know how to identify the biofilm and only by sending the entire ulcer to next generation sequencing are we going to be able to identify things we might be missing.
Melissa: Can you just explain what resect means for people that don’t understand?
Dr. Hlavinka: Resect means to remove by surgery and typically when you do that with a scope you have these instruments that basically, well, they’re kind of like they’re kind of like gougers. They just go in and sort of gouge something out like you’d scoop out of a melon, you know scoop a little scoop out of a melon – miniature versions of that.
I hate to be crude but believe me, if you got it done by me I’d explain a lot more in detail and get you through it. And really, they’re small, they’re small devices and they’re small ulcers so we’re talking about no more than about the skin of your pinky knuckle. That’s about the biggest piece of tissue you’d resect.
Melissa: Is it a painful procedure for the patient?
Dr. Hlavinka: Pain is subjective from a standpoint of the patient and the provider so I’m someone who’s exquisitely sensitive to pain because I’ve treated chronic pain patients my entire career and I realized how horrible we medical providers have been to people with chronic pain. I apologize for all the horrible stories I’ve heard.
My very best friend has had chronic pain after cancer chemotherapy and has lived with it his entire life so I know the truth. And I know that all the opioid addiction is once again a very sad way for docs to pass the buck.
What I do is I do something beforehand. I inject the ulcer with a needle called a Williams needle, through a scope with a local anesthetic in the area. So it’s like if you had to have something in the dermatologist and they would numb underneath it and then resect it and then sew it up.
I’d do that first, so that sort of helps the pain because before the resection and then I put a solution in the bladder with the long-term antibiotic. I should say a long-term analgesic and numbing medicine and a bladder anti-irritant and I leave that in for an hour while the patient’s waking up from recovery. Then I take it out and that that helps. That helps but I’m not saying it makes it pain-free.
But by and by I believe pain can be decreased. Also I use B&O suppositories Belladonna and Opium suppositories, an ancient urologist trick that decreased spasm. I get one of those before they wake up in the recovery room and you do all sorts of things to diminish it but I think it depends on the patient’s pain scale. If a patient has a high pain scale they’re probably going to have significant pain with this resection.
Multiple Organisms – Indicator of Biofilm?
Melissa: Okay that’s good to know. So there are two directions that I want to go in. One is further down the IC treatment path, but I also want to ask a couple more questions about biofilms.
You’ve mentioned NGS as a way to actually do testing to maybe pick up multiple organisms. Is seeing multiple organisms on test results a potential indicator that a biofilm is present?
Dr. Hlavinka: Absolutely yes. If you have multiple organisms and NGS tells us that, then my opinion is that’s a strong indicator of a biofilm.
Melissa: From a patient perspective again, when they’re trying to identify whether biofilm may be involved, if taking antibiotics brings relief but the symptoms always return when the antibiotics are ceased, could that also be an indication that there’s some kind of biofilm involved in the bladder?
Dr. Hlavinka: Yes. The reason is, is that failure to eradicate an infection despite appropriate antibiotics, and again appropriate antibiotics is indicative of a complicating factor and that can be something as significant as a foreign body – a stone, an ulcer – and in my opinion a brand new topic of biofilm. And honestly, Melissa, I feel like we haven’t even begun to touch the surface.
For instance in males and prostatitis I’m convinced that there are multiple micro-biofilms in the body, I should say in the prostate. The prostate is like a lung with a little alveoli, little lung pockets that we breathe through. All the little tiny glands in the prostate that produce semen, in my opinion there’s probably dozens of different micro-biofilms in those that could be explaining, and maybe one is stronger, you know, one is predominant today and next month another one’s predominant.
So you could repeat it and them be different. And I’m convinced that say for instance if I look in a lady and she’s got 20 of these little pustules in there, these little pimples in the bladder, who’s to say that there’s not 20 different biofilms micro-biofilms and each one of them might be different.
Now from a practical standpoint you’re not going to biopsy all of them because that’s just too much trauma to get the answer, but you might start learning to biopsy three to four to five and that’s what I’m going to do in the future.
If you’ve found this information helpful, you can support future expert interviews and other projects by contributing to the work that means the most to you. To become more actively involved, become an official Live UTI Free member.
Acknowledgments
Discussion around the vaginal microbiome, biofilms, and probiotics and UTI occurs frequently, and the information is sometimes debated. While more research into each of these topics is needed, we’d like to thank Dr. Tim Hlavinka for giving us the opportunity to learn of his experiences and helping us develop a better understanding around these topics.
More from our expert video series
Watch the rest of our video series with Dr. Tim Hlavinka, or subscribe to Live UTI Free on YouTube.
- UTI And Hormones, HRT And Contraception
- How Is Interstitial Cystitis Diagnosed?
- New Treatments For Interstitial Cystitis, UTI And Prostatitis
- UTI And Sex: Should I Get My Partner Tested?
- UTI And BV, Yeast Infection And Other Risk Factors
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions in the comments below, or reach out to our team directly.