UTI And Hormones, HRT And Contraception
UTI and hormones are linked, and while the research into exactly how is somewhat lacking, we hear from people every week who have experienced this link firsthand.
In this video, Dr. Tim Hlavinka discusses the connection between UTI and hormones. He also delves into the relationship between hormone replacement therapy (HRT) and recurrent UTI.
The discussion on hormones extends into the various contraceptive methods and how birth control pills, IUDs and other forms of contraception may have a direct or indirect impact on bladder health.
Watch the video to learn more, or read the full transcript below.
Jump To Section:
- Video 1 Transcript: UTI And Hormones, HRT And Contraceptive Methods. >>>>
- UTI And Hormones – Is There A Link? >>>>
- Preventing Menstrual Cycle Linked UTI. >>>>
- UTI And Hormones: When Is HRT Beneficial? >>>>
- UTI And Hormones: Can Vaginal Rejuvenation Help? >>>>
- Could An IUD Cause Recurrent UTI? >>>>
Video 1 Transcript: UTI And Hormones, HRT And Contraceptive Methods
Melissa: Today we’re talking with Dr. Tim Hlavinka, and I wanted to ask you first if you can give us a little background about your professional career and how you became interested in women’s health?
Dr. Hlavinka: Thank you, Melissa and welcome. I began my urology career 30 years ago. Board certified in urology in the U.S. since then. I’ve always had an interest in urinary tract infections just because I had an interest in microbiology in my undergraduate and graduate studies.
I’ve always been fascinated by infections and microbes so it was natural for me to be able to select this as part of a subspecialty when I got into urology. And secondarily I did reconstructive surgery and urology for about 20 years, doing over 200 major reconstructive cases.
All of those patients, almost all have complicated urinary tract infections. And indeed with that population starting out as young as age nine when I operated on them, now my oldest patient in that practice is 31 and has had a baby. I needed some answers for infections. I was the go-to person for complicated infections since all of my patients had complicated infections.
Then that started encompassing pelvic floor issues, incontinence, hormone related urinary tract infections. When I saw the fact that we couldn’t help most women prevent infections and it was simply a hormonal deficiency then I began to become interested in women’s health and women’s sexual health because of the frequency of sexually related infections in women.
So I started my career as a female sexual health and women’s health specialist in 2003 and I’m a member of the International Society for Women’s Sexual Health and a fellow of that organization.
It’s a very good organization that’s multi-disciplinary and absolutely non-biased by pharma and unbiased by patients. So it’s a very good resource for information, much like the North American Menopause Society and I believe it’s called the European Menopause Society, that version of that.
So because of that specialty and subspecialty, pretty much infections have been a big part of my practice forever. And the frustration at not being able to eradicate an infection and lately the frustration at not being able to even identify if something, a given set of symptoms, came from an infection, has been a part of the sort of chronic irritation in my white doctor’s collar for forever.
And so because of that I have always explored new ways of detecting and treating infections and have been open. When you’re the buck stops here type doctor you don’t get to say well go see somebody else. You’ve got to look at alternative therapies, you’ve got to look at contributing factors, you’ve got to look at any information that’s going to give you an answer for your patient. And that’s why I’ve evolved to where I am now with the next generation sequencing testing.
UTI And Hormones – Is There A Link?
Melissa: Well that’s excellent because we’ve collected a couple of hundred questions from our audience and I thought we could just start with the hormones and hormone replacement therapy angle of recurrent UTI. And so if you don’t mind I’ll just start asking you some of the questions that our audience submitted.
Dr. Hlavinka: Absolutely.
Melissa: First maybe you can talk about whether there is a link between hormones in recurrent UTI in premenopausal and post-menopausal women?
Dr. Hlavinka: Yes, there is definitely a link there is a link at all, all the spectrum of the hormone life of a woman. We know that infections tend to happen, I should say an increased risk of infections tend to happen at those milestones hormonally in women. At the time of the first menstrual period, the time of becoming first sexually active, the first pregnancy, obviously perimenopause and the menopause. There’s always a spike in infections at that time.
So clearly the observation that hormone fluctuations has something to do with a woman’s susceptibility to infections has been information we’ve known for 70 years. But we really didn’t have a means of treating it. And that sometimes is not a deficiency as much as it is a fluctuation in the hormone level, particularly when a woman is cycling or coming off a pregnancy when she has estradiol levels of 5000 and they drop down to 30 for instance if she is breastfeeding.

So these are the kinds of things that we see. And so I would answer the question, is there a link between HRT and I should say between hormones and those phases of a woman’s hormonal life? Absolutely. Absolutely. And we can get into all the details of why that happens later on.
Hormone Replacement Therapy (HRT) And UTI
Melissa: Okay. So you said there is a link between hormones and UTI and then you mentioned briefly HRT and UTI. Maybe you can explain that link a little more?
Dr. Hlavinka: So you can see someone getting better with hormone replacement therapy. Alternatively, a rare woman will get worse simply because the microbiome is upset by a different set of hormones that her tissues are used to seeing. And so I try to tell patients that when you’re coming in with hormonal issues, let’s say the most common one would be the perimenopause.
A woman’s 49, starting to have irregular periods, starting to have maybe some other symptoms of menopause like hot flashes or sleep disturbance, low libido, all sorts of things like that. Vaginal dryness, well that’s a sign. That’s the canary in the coal mine that menopause is imminent.
My problem is that my colleagues wait until somebody’s had their last period for 12 months to call them menopausal. Well, it’s an epidemic now, Melissa, of early perimenopause. I just started a 39 year old on full hormone replacement therapy. She has both ovaries, never had any other kind of issues, no sickness, chemo, nothing and she’s full-blown menopause at 39.
It is not uncommon at all and we will get I think the question – I may as well take it right now because there’s a form about the contraception. It is not at all uncommon for very young women when they’re taking strong and even lower dose oral contraceptive agents to have a profound diminishment in their estrogen. The contraceptive gives your body enough estrogen to fool it into not ovulating but not enough to have nearly what you need for estradiol replacement and progesterone replacement at that phase of your life.
And so the common practice in the United States and throughout the world I’m so told is to give these low-dose oral hormones (and we’ll get into detail why that’s really bad) at the time of the perimenopause just to kind of calm down symptoms. It’s the worst possible thing you could do because the oral hormones are the worst form and they actually exacerbate many of the problems of the perimenopause.
So my youngest who came in on oral contraceptives since age 14 was 21. Full-blown menopause at age 21. I mean, not just vaginal dryness but she had vaginal atrophy that you couldn’t get even a pinky finger in her vagina at age 21.
It took me 18 months of aggressive hormone replacement therapy and vaginal dilation and stimulating her ovaries to get her back. And she did call me and tell me that she had a healthy baby at age 27 so I’m really satisfied with her, but it is not at all uncommon to see full-blown menopause at age 35.
Mark my words, take this to your providers – if they’re not aware of this, they need to be. There are seven percent of women – in one out of 14 there is actually a genetic alteration on the androgen, the male hormone receptor, that makes you susceptible to premature menopause from as short as six months on the pill, all right. And it doesn’t matter if it’s low dose, high dose.
So there’s that group of women that are going to be on the pill for six months and they’ll never be the same. Their hormonal trajectory throughout life will be downward and they will be the ones that come in at age 35 already complaining of menopause.
Birth Control And Pre-Menopausal UTI
Melissa: Is it possible to look for that gene before going on birth control?
Dr. Hlavinka: I keep trying to get my colleagues with how inexpensive it is to create genes these days, why hasn’t someone? That should be a panel of every woman who comes in for her first pap smear or first pregnancy test, so yes i will bring that up again. I’m glad you said that because if it’s patient driven sometimes they’ll listen.
It can’t be a cost factor anymore. So that is something I think that women need to be recognized and be proactive because so many women’s health providers are so happy that women have control over their reproductive processes that they’re willing to take the side effects so to speak.
And in the past when that was predominantly male providers, I can see how awful that is, but that is across the gender spectrum in medicine providers, I just believe it’s just so easy to give a woman a pill and not worry about it and not worry about the detritus that may happen afterwards genetically, or physiologically. So that’s my take on that.
Melissa: Okay, when it comes to people who are menstruating and are not on birth control, can you explain more the mechanism of infection that happens at certain times of the cycle?
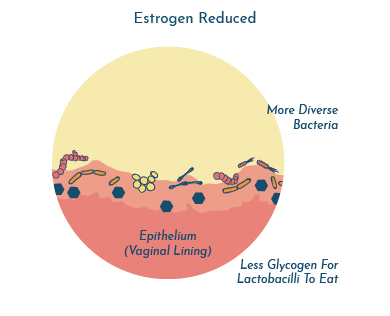
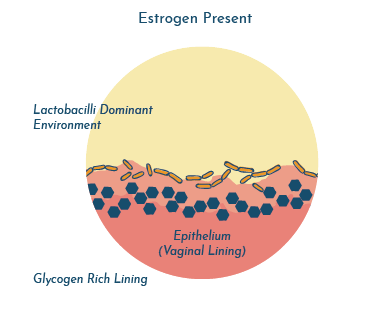
Dr. Hlavinka: So you have your peaks and valleys during the menstrual cycle. You have your phase where the uterine lining is being built up. You have your pre-ovulatory phase where there’s a surge of testosterone and estrogen, and that of course is when there’s less susceptibility to infections, simply because everything’s all protected.
But of course that’s when the woman has intercourse, and so sometimes that’s when she does get them because she may be ovulating or periovulatory.
And then you have a rapid decline with the menses and the menstrual bleeding and you get a low ebb of the hormones at that time before you build back up. So at both of those time frames, just because she’s more likely to be having intercourse because of the higher libido associated with ovulation, and at the other part of the cycle where the hormones are low.
And you can actually have subtle changes in the physical chemistry of the vagina. The microbiome changes over the menstrual cycle and thus the susceptibility to infections does.
Same thing with the vaginal epithelial layer. The vaginal lining layer undergoes profound changes throughout the cycle, becoming more sensitive and susceptible at the low ebb and less sensitive and susceptible at the higher. But again you have that confounding factor of if she’s having intercourse, okay?
Preventing Menstrual Cycle Linked UTI
Melissa: We do hear from a lot of people that say they experience UTI symptoms right before their period. Is there anything that you can do to kind of stop that from happening?
Dr. Hlavinka: It is possible to prevent the infections or the bladder irritation that happens right before a woman begins her cycle. I tend to do non-hormonal approaches to that and more practical ones. To take more aggressive doses of probiotics during the three or four days before your menstrual cycle will happen – the bleeding portion of the menstrual cycle. Sometimes you can take some of the urinary antiseptics and things like Cystex or Mandelamine to kind of prep the bladder to not get infected.
Also, being very careful about avoiding any sort of irritants, vaginal irritants and things like that. You know things like spermicides or any sort of douching or something like that. Be very careful about the cyclical changes that happen, to prevent the irritation that might happen at that time.
Melissa: One other question on that topic then: If it is a cycle of hormones that is causing this irritation is it necessary to treat those symptoms or will it cycle back up?
Dr. Hlavinka: I would say that it is not necessary, it just depends on the bother. That’s a difficult one to categorically answer, Melissa. I would say if it’s really bothersome and a woman’s worried that she may have urinary tract infection and feels like running to the provider to check a urine every time and that becomes an issue, then I would be more aggressive. Otherwise, in my opinion, we say in urology the solution to pollution is dilution – lots of water and things like that.
UTI And Hormones: When Is HRT Beneficial?
Melissa: What are some of the indications in perimenopause and menopause that hormone replacement therapy may be beneficial?
Dr. Hlavinka: My opinion is that symptoms are the most important thing. And I cannot get my colleagues to understand how in depth a hormone deficiency may be and how much risk that puts a patient in, because it is not treated and not treated aggressively.
So when it’s something like recurrent urinary tract infections and we have options, it’s easy to kick the can down the road and put a woman off when the background may simply be hormone replacement therapy. I should say, the background therapy should be hormone replacement therapy.
Much like if you’re trying to paint a wall. If you don’t put a primer layer on you’re not going to get the paint to stick. And then none of the other therapies will be effective. So having said that, I am constantly almost universally surprised at how little in depth my providers, my colleagues that do women’s health go into detail about what might be menopausal symptoms.
For instance, unless they’re just having full-blown hot flashes and miserable night sweats, they ignore them. Well, for me a loss of vertebral, a loss of a half an inch, well she’s probably got osteoporosis and nobody’s done a DEXA scan.
Vaginal dryness, well, that means that she’s had a hormone deficiency in her vagina that’s going to put her at risk for trauma during intercourse and recurrent urinary tract infections for at least a year once you first start noticing dryness.
The other thing, it’s just a change in skin. Estrogen is, I should say, a woman’s skin is so sensitive to estrogen levels and just coming in and saying my skin is dry doctor it really just doesn’t look the same to me. Those are the subtle signs I’ve seen over the years.
At least measure. And sure you can say you’re perimenopausal, there’s nothing we can do. That’s the most incorrect thing that’s possible. It’s just hard to treat a woman when she’s perimenopausal and so nobody wants to do it. Or they want to give them the pellets that we’re doing so much in the United States here, where you know everybody’s getting these pellets in their rear ends and they’ve got super physiologic hormone levels and they’re happy but nobody is looking at the long term. Now that may be a good thing.
Maybe these women are going to be better off as they age with the higher levels but we just don’t know that and so individualizing a woman’s evaluation and individualizing a woman’s therapy are the absolute essentials if you’re going to do women’s health.
You just can’t do it any other way and to think you can do it effectively, to do it ‘my way’? That doesn’t work because almost always ‘my way’ isn’t her way.
Melissa: I 100% agree with that. So is it possible to reduce or eliminate all symptoms of menopause and should you even aim for that?
Dr. Hlavinka: It’s a very good question. Well, I would say that depends on the woman, because some of them absolutely insist on that and others are okay with changing the sheets every night because they sweat through them.
I believe that a woman should not suffer with the symptoms of menopause. That is an indication that the estrogen deficiency is too profound.
And again unless we’re doing things like bone mineral density and looking at subtle signs of estrogen deficiency, you don’t know the long-term impact. But my opinion is also that what if vaginal dryness and pain on intercourse and recurrent urinary tract infections is a trigger and a canary in the coal mine, as I said, for estrogen deficiency elsewhere that you don’t see.
Maybe that’s brain and protection for cognitive decline. Maybe that’s bones, maybe that’s skin, maybe that’s all sorts of other tissues that have more need for estrogen. Because I can tell you I had women come in at age 38 and have osteoporosis and they look 28, and that’s the only part of their body that needs more estrogen. The rest of it isn’t going to need estrogen for 20 years or more.
And so if we don’t look at those women we’re not going to find the kind of key components of the menopause transition that may need to be treated 10 years before menopause for instance now.
And in fairness, we don’t have a lot of markers for that. We we need more work in that area to look at some biomarkers and things like that would help us to predict in these women – much like that androgen receptor for use of the pill. Those are the kinds of things we need to have developed.
What Does HRT Involve?
Melissa: Can you explain a little bit more what hormone replacement therapy typically looks like? Is it a balance of hormones or is it a single hormone? Is it different for everybody?
Dr. Hlavinka: It should be different for everybody because not every woman needs the same. To be specific we should go into pre-menopausal, full-blown menopausal and with and without a uterus because those are four major categories of therapy. And the easiest woman to treat is a post-menopausal woman who has had a hysterectomy because then there really is not a need for progesterone. That’s very, very controversial. There are some that find that progesterone is essential for things such as mental health.
For instance, a woman that has post-menopausal headaches, I almost always include progesterone because it does have sort of a neural calming effect. There are women who have sleep disturbances that the progesterone helps for. Certainly there are women who need progesterone but to say, like a lot of my colleagues, that every woman needs progesterone no matter what I think, that’s treating them their way and not the way the patient needs it.
Because let’s face it, progesterone is the one that kind of makes you bloat and gain weight. And the fluid retention and the kind of lousy symptoms, that sort of premenstrual syndrome symptoms of you know feeling bad and the mood changes – progesterone is all part of that.
UTI And Hormones: Is HRT Safe Long Term?
Melissa: How safe is it to be on HRT? Can you take it long term or should you try to taper it off at some point?
Dr. Hlavinka: So the whole notion that the shortest amount for the, I should say, the lowest amount for the shortest time to treat symptoms, that was once again – and hopefully we have learned in the modern post-COVID era that scientists and doctors are full of policies – they like to parade them as science but they’re full of policies and that was a policy by the North American Menopause Society based on a study. The women’s health initiative that scared the heck out of everybody.
That study was preeminently flawed. It was one of the most profoundly damaging events that happened in the long history of sordid issues and treatment of women and women’s health. So to undo the damage, that’s taken about 15 years.
So I have 88 year olds who wring me by the neck if I don’t refill their hormone replacement therapy and I have younger women who have difficulty with HRT. Perhaps there’s a side effect that’s bothersome or we just can’t quite get the levels right and they elect not to have it.
But what is known and what is clear is that within the first two years of menopause and for 10 years, and again if you have menopause at age 42 this is not the same as a woman’s average menopause at age 51, you need to continue that for 10 years afterwards.
There’s clear data that the hormones are physiologically protective during that time frame. And again, let’s look at medical studies. Medical studies don’t take a woman across the spectrum. They cut you off at 49, at 59, at 69, at 79. So the whole data is linked to decades of life, but you don’t have a magical change between 49 and 364 days, and you know, 50 and one day, all right? That doesn’t change that fast.
So we have to think. And we have to think about that, and so for a lot of women I think it’s lifelong and it should be because there’s going to be a good cardio protective event – there’s going to be cardio protective aspects of it. There’s going to be bone density, mental capacity, muscle maintenance, all of these things for a woman. I think it’s important to continue that on. And we don’t really have an answer.
We do know that in the first decade afterwards for instance, that it is protective. There is actually a lower incidence of breast cancer in women who took it – lower. I didn’t say equal, I said lower. And again, you can’t say that hormones are safe and you’re not going to get breast cancer. It takes me 20 minutes of history, just history, (and that doesn’t involve laboratory exam) and discussion.
My appointments for a woman to start hormone replacement therapy are twofold. The original one to get the information for 45 minutes and the second one for an hour and 15 minutes, to be able to decide what therapy she needs safely and to discuss the side effects. So I take two hours with these women to find out what they need and you can’t do it in any shorter than that.
Different Types Of HRT
Melissa: We did receive a question about newer types of hormone replacement therapy, so bioidentical hormones, patches and creams and other things that are coming onto the market. Do you see that those are actually safer or more effective than more conventional types?
Dr. Hlavinka: In my lectures on hormone replacement therapy I have a big slide that says all these terms and basically attacks them. The most important thing is to have a bioidentical hormone. The closer that little molecule, that estradiol, that progesterone, and that testosterone, the closer that is physical chemistry wise to a woman’s own hormones, the safer and the better and the more effective it is.
And the reason is, is that all hormones get changed in the body. They get metabolized primarily in the liver and the breakdown products are some of these. For instance Premarin.
Premarin is the worst possible one we could possibly have and you know where that came from? Pregnant mare urine. Wasn’t that real clever? That’s where Premarin comes from – pregnant mare urine.
So that in and of itself is such a sexist term. Oral Premarin is the scourge of my existence and makes my job very hard. But to say bioidentical, okay, how do you get bio-identical?
Natural, so natural comes from natural sources. That would be the pregnant mare’s urine. All right, so Premarin could be natural but it is certainly not bioidentical. You can get estrogen and progesterone and testosterone from yams and you can get it from soy and you can get it from other products, but you have to go through a chemical degradation project, I should say, you have to go through a chemical degradation process to get it to its forms that you can make it into something that can actually be safely used by a woman in a cream or a pill.
But by and by, the fact that something happens when you swallow a pill, and even the sublingual, and even the dissolve in your mouth troches – those have some first passage effect through the liver and creation of metabolites that we don’t understand and we can’t measure that are certainly behind a lot of the complications. The blood clots, the weight gain, the liver
issues and what I’m convinced of, the higher incidence of breast cancer. All of those things are because of the metabolites that go there.
So definitely in the vagina and on the skin are safe and a cream and a patch is much better. Whether or not pellets is okay and safer I don’t really want to get into the weeds of that one, but a lot of people are getting them and done by the right provider they are safe. My parent organization would say that’s controversial and I will say I agree with them, it’s controversial. But many people, many good quality providers, including myself, use them.
Melissa: Okay, and someone did ask whether it’s safe to use an estrogen cream on a daily basis, long term?
Dr. Hlavinka: If we’re looking at an estrogen cream in the vagina and on the external genitalia this is a good place to segue into one aspect of that. And one of my pet peeves and how it’s given. Yes, it’s safe to use for the lifetime. Many women have to. I have many women, who if they stop their estrogen cream for three weeks, UTI, incontinence, vaginal dryness, comes right back.
So for some women they can build up their lining layers – so let’s talk about the vaginal creams first. And again, all are the same from the standpoint, the vaginal troches, vaginal suppositories, the little pills like Vagifem and things like that.
Although, Vagifem is so weak these days. It used to be 25 micrograms, it’s now 10 micrograms, so honestly, you should be taking it every day. But three times a week, one gram deep in the vagina, of estrogen cream is the right way to do it and then a second half a gram spread on the external genitalia and the urethra. They’re actually are, deep in the vagina, predominantly estrogen receptors. As you get to the mid-vagina and even the external genitalia, testosterone, androgen receptors become more common, and those androgen receptors are very important.
Now, most women that are getting testosterone replacement get enough to satisfy the receptors in the vaginal and genitalia area. The clitoris for instance is 100 percent testosterone sensitive, almost 100 percent androgen receptors. And that’s why it can be a side effect of testosterone replacement therapy in women, is clitoral enlargement.
But I think many providers don’t realize that, and they tell them to smear it on the external, take a half a gram and put it on your urethra at bedtime.
Well that’s worthless. Number one, it’s going to wash off. Number two, you’re gonna urinate the next time and wipe it off. If you don’t put it deep in the vagina where the estrogen receptors are, you’re not going to capture it and it needs to be done at least three times a week, one gram, and a half a gram of external genitalia. Whether or not you need a combination of estrogen and testosterone cream, which I use in a lot of my patients when they’re really not getting the responses.
Again, some women are more susceptible. Some women don’t need the testosterone portion of it. Some of them are exquisitely sensitive to a lack of testosterone in the external genitalia. They need it to maintain external genitalia health.
UTI And Hormones: Can Vaginal Rejuvenation Help?
Melissa: Okay. So there is a question on vaginal atrophy and the rejuvenation procedures. Can you comment on that and maybe give us a bit more insight into how they work or don’t work?
Dr. Hlavinka: The first thing I do for a woman when she comes to my office, because I do those treatments, is I do the radio frequency device. I also use the platelet-rich plasma, the so-called o-shot, which yeah, it does work. It does work for that.
And a lot of women love it, but the first thing I do when a woman comes to me for a consultation is I take a history about hormone replacement therapy and about menopause in her family history. Do women have early menopause? How about vaginal dryness? Pain on intercourse?
Do you need lubricant? You know the problem with lubrication is that the quantity of lubricant may be fine for a woman, even a woman many years after menopause they are responding to the sexual response by creating a lubricant, but the quality of it decreases. So clearly the relationship between adequate estrogen levels and the quality of lubricant and therefore the protective aspect of that is as much less as a woman gets older.
So having said that, the most important thing to recognize is that continuing to do that is important. It’s very important that if you’re going to have a rejuvenation procedure that you have adequate vaginal estrogens and unless a woman’s under 40, I pretty much give them six weeks to three months of vaginal estrogens and tell them to come back. Many times they’re happy with things, but afterwards it makes me more successful because those are healthier tissues and my vaginal rejuvenation is going to work on healthier tissues.
Is The Mona Lisa Effective For Vaginal Rejuvenation?
Melissa: That makes sense and the particular one that a lot of people mention is the Mona Lisa. Can you comment on that?
Dr. Hlavinka: Unfortunately, in the U.S. there was a moratorium put on these devices. There was a black box warning. Seven companies got named. The company that has my machine, that sold me my machine, does too and that was a real problem because it’s an extremely safe device.
We vetted it for months. We did trials. We tried the Mona Lisa, we tried the cynosure laser. We tried our device. I’m not going to say companies. I don’t want to say who’s better or who’s not, but the bottom line is that you have to individualize.
The problem with this, is the laser is very superficial and for women who have genital urinary syndrome and menopause or vaginal atrophy, it does work well for that, but in my opinion it did not treat the deeper layers as effectively. And indeed, the ThermiVa device, same thing, it just wasn’t that strong. Now, there may be devices on the market that are superior now, both laser and non-laser devices.
The bottom line is that you need to deliver energy to the tissue to create the kinds of changes in the architecture and if you don’t deliver adequate energy deep, you’re not going to get any benefit from it. So I’m not a big fan of the Mona Lisa.
UTI And Hormones: Could An IUD Cause Recurrent UTI?
Melissa: Before we leave the topic of hormones and hormone replacement therapy, I just wanted to ask around different forms of contraceptives. You’ve kind of touched on the fact that a hormonal contraceptive could be linked to recurrent UTIs, just because of the change in hormones, but what about devices like an IUD, whether it has hormones or not?
We’ve actually heard from quite a number of people over the last few years that associate the onset of their recurrent UTIs with the insertion of an IUD. Do you see that, and do you have an explanation for why that could happen?
Dr. Hlavinka: I see it weekly, at least weekly. I guess that makes it pretty possible if I see it weekly. I think, like I said, when there’s any changes in a woman’s architecture, that can change the microbiome.
Perhaps there is a difference in the excretion from the cervix and that subtle change, I mean these are exquisitely sensitive environments, micro environments, and under those circumstances it doesn’t take much to change.
I have seen that whether it’s a hormonal or non-hormonal IUD, in just the placement. I’ve also had a lot of women who get off the oral hormones and that’s been the best thing for them because they don’t have the estrogen suppression and they finally get healthy tissues. So I would say it again has to be tailored. There’s not a perfect solution for women, unfortunately.
Some will have problems with the IUD, some will have, certainly many will have problems with the pill. And under those circumstances it’s individualization.
The non-hormonal IUDs are preferable simply because the hormones that they elute, even though they’re safe and they’re absorbed into the vagina, I should say in the uterus from the vagina, I should say they’re directly absorbed in the uterus, they’re still a micro environment. There’s still a circulation around there where the pelvic circulation gets affected. And so you just can’t say. And there’s pretty good data to show that the Mirena can affect hormone levels too.
If you’ve found this information helpful, you can support future expert interviews and other projects by contributing to the work that means the most to you. To become more actively involved, become an official Live UTI Free member.
Acknowledgements
The topic of UTI and hormones comes up a lot in conversations with our community. Many people describe this link, and we hope that future UTI research will better address it. We’d like to thank Dr. Tim Hlavinka for generously sharing his time to answer the questions submitted.
More from our expert video series
Watch the rest of our video series with Dr. Tim Hlavinka, or subscribe to Live UTI Free on YouTube.
- Probiotics And UTI, Biofilms, And The Urinary Microbiome
- How Is Interstitial Cystitis Diagnosed?
- New Treatments For Interstitial Cystitis, UTI And Prostatitis
- UTI And Sex: Should I Get My Partner Tested?
- UTI And BV, Yeast Infection And Other Risk Factors
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions in the comments below, or reach out to our team directly.
