Chronic Urinary Tract Infection vs. Recurrent UTI
Is a chronic urinary tract infection the same thing as a recurrent UTI? What does it mean if you get frequent urinary tract infections or have continuous UTI symptoms? Is there anything you can do if you keep getting UTIs?
These are just some of the questions we get on a daily basis. Below, we’ve answered these as best we can. We hope that after reading this, you’ll better understand what may be happening in your own body. And even better, feel more equipped to tackle it head on.
Jump To Section:
- Persistent UTI vs. recurrent or frequent UTI: what’s the difference? >>>>
- Why do I keep getting UTIs? >>>>
- The different types of chronic urinary tract infection. >>>>
- What causes chronic urinary tract infection (aka frequent UTIs)? >>>>
- Can you test for chronic or frequent UTI? >>>>
- When to see a doctor for chronic urinary tract infection. >>>>
Persistent UTI vs. Recurrent Or Frequent UTI: What’s The Difference?
 | A recurrent urinary tract infection is officially defined as three episodes of a UTI in the previous 12 months or two episodes within the previous 6 months. |
At the moment, it is generally accepted that recurrent UTIs occur due to either reinfection or a persistent infection.
 | Reinfection refers to an infection where the pathogen is eradicated by treatment, then the same or a different pathogen ascends the urinary tract to cause a new infection. |
 | Persistence means the pathogen that caused the UTI is not completely cleared from the bladder by treatment, remains detectable in the urine, and after treatment returns to a level that once again causes symptoms of infection. This cycle of persistence can repeat indefinitely, feeling like a new infection each time. A persistent infection is also called a chronic urinary tract infection. |
Evidence suggests that many recurrences of UTI may actually be caused by an underlying bladder infection that came about due to ineffective initial treatment.
Frequent UTIs caused by persistent bladder infection are also referred to as chronic cystitis or chronic urinary tract infection.
Note that while terms used for various urinary tract conditions may sound different, they could refer to the same thing. Check out our interview with Dr. Lindsey Burnett who shares insights on the clinical difference between acute, recurrent and chronic UTI.
When we refer to recurrent UTI in this site, we usually mean persistent infections; also called chronic urinary tract infections.
If your frequent UTIs are actually caused by an underlying chronic urinary tract infection, you need to pay attention here:
Whatever you’re doing to treat each occurrence of UTI is probably not working.
The fact that your UTIs keep returning should be enough evidence of this. But you may not know why chronic urinary tract infections are so hard to properly treat. Fortunately, we can explain it through super interesting science.
Why Do I Keep Getting UTIs?
While most uncomplicated UTIs either resolve on their own, or with a course of antibiotics, there is an increasing number of cases of chronic urinary tract infections that cause ongoing symptoms.
You get a UTI, you take the antibiotics you are given, the symptoms disappear, and everything seems normal. Then you suddenly find yourself with another UTI… You take the antibiotics you are given, the symptoms disappear, and everything seems normal, until…
It may sound like a broken record, but this is the situation more and more females find themselves in. To hear personal accounts firsthand, listen to UK reality TV star Marnie Simpson discuss her UTI experience and being misdiagnosed with recurrent UTIs.

“I’ve had recurrent UTIs for around 15 years. I take antibiotics when it gets really bad, and it seems to help, but I always get another one, and I always anticipate getting another one. I try my best to prevent it, but it seems inevitable.”
Statistics Around Frequent UTIs
While the statistics around chronic urinary tract infections are hard to find, we do know that:
- 30-44% of females with an initial UTI will experience a second UTI. And with each UTI, the risk of another UTI increases.
- Frequent UTIs may be caused by multiple organisms simultaneously.
- A significant proportion of our quiz respondents have suffered 7+ UTIs, with a recurrence every 1-3 months.
- Our own data indicate that most females who experience recurrent UTIs do so despite standard antibiotic treatment.
- Testing and treatment guidelines for chronic urinary tract infections are inadequate or do not exist in most parts of the world. This means even when doctors want to help, they generally don’t have the resources or guidance they need to be able to.
- One study found that 74% of females diagnosed with Interstitial Cystitis had previously been diagnosed with recurrent UTIs. Interstitial Cystitis (defined below) is a painful set of urinary tract symptoms with no identified cause and no known cure.
- 93% of the females included in the above study had also received negative test results after having their urine cultured (more on this in our testing guides).
In short, a significant number of females move through escalating stages of diagnosis as antibiotic treatment fails to cure them and testing fails to find a cause.
The Absence Of Recurrent UTI Guidelines
Because there are no guidelines on managing complex or recurrent UTI, primary care doctors are generally not in a position to help.

“Most UTI guidelines are aimed at management of simple uncomplicated UTI. It can be very difficult to successfully manage complex or recurrent UTI in primary care. If symptoms persist, or where there is diagnostic uncertainty GP’s will need to make a referral for specialist assessment."
For females that progress from a single UTI, to recurrent UTI or chronic urinary tract infection, or to a diagnosis of Interstitial Cystitis, there has historically been very little hope of effective treatment. We hope to help change this.
Different Types Of Chronic Urinary Tract Infection
Depending which country you are in, what your symptoms are, and which terminology your doctor is familiar with, you may have heard the following terms to describe different conditions of the urinary tract:
Chronic Urinary Tract Conditions: Different Names For The Same Family Of Problems
| Acronym | Term | Definition |
|---|---|---|
| RUTI | Recurrent Urinary Tract Infection (Specifically, persistent recurrent infections) | Three episodes of a UTI in the previous 12 months or two episodes within the previous 6 months. RUTI can be classified as a persistent infection or a reinfection. The open nature of this definition means there is no logical end to this diagnosis. Even after twenty years of UTIs, this definition can still apply to you. |
| cUTI | Chronic Urinary Tract Infection / Chronic Cystitis | A persistent infection of the bladder. As with RUTI, many females are diagnosed with chronic cystitis indefinitely. |
| IC PBS BPS | Interstitial Cystitis Painful Bladder Syndrome Bladder Pain Syndrome | An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes. |
| HBS HSB | Hypersensitive Bladder Syndrome Hypersensitive Bladder | An umbrella term used in East Asia to cover conditions resulting in symptoms including, bladder pain, discomfort, pressure or other unpleasant sensation, and is associated with disorders such as a frequent need to urinate day and night and/or an urgent need to urinate. It encompasses Bladder Pain Syndrome. International Painful Bladder Foundation |
If you do a little research, you will quickly find there are also sub-categories within these conditions, with varying symptoms and levels of injury to the urinary tract.
It is not our intention here to imply these chronic urinary tract conditions are the same, or that they affect people in the same ways. But they do have an important thing in common – in the majority of cases, no cause has been identified, and the condition is therefore not curable. Treatment focuses on reducing symptoms rather than resolving the underlying issue.

“After about 3.5 years of chronic urinary tract infections, two doctors said they couldn’t help me further. A third said ‘maybe you just have irritable bladder or IC.’ That ‘maybe’ didn’t feel like a diagnosis. Why did my test results tell them nothing?”
So why do we mention these chronic urinary tract conditions?
There is strong evidence that many have been misdiagnosed with incurable conditions, when in fact they are afflicted with a chronic, embedded bladder infection that can be identified with appropriate testing, and treated effectively over time.
Let us explain…
What Causes Chronic Urinary Tract Infection?
This is where the science gets a little more complicated. (But fascinating too!)
We’ve talked elsewhere about what causes UTIs. And above, we explained that recurrent UTIs can be attributed to a persistent bladder infection that is not properly eradicated by treatment.
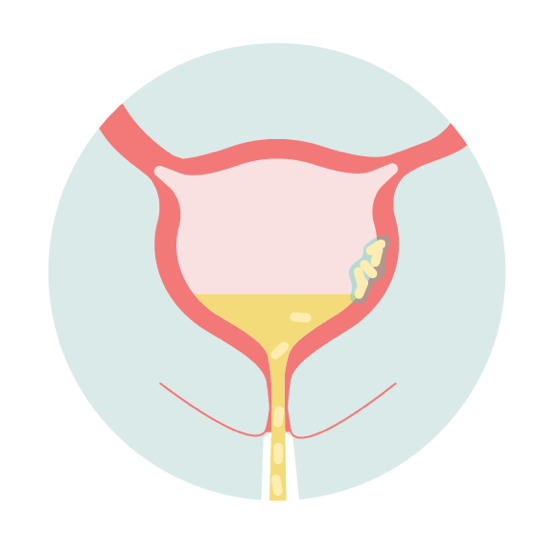
A persistent bladder infection can last for years in the form of a chronic urinary tract infection. For many females, the cycle of acute and symptom-free periods is never broken, and some move on to be diagnosed with the conditions mentioned above, such as Interstitial Cystitis (IC), or Painful Bladder Syndrome (PBS). More on that later.
Why has it been so difficult to detect and treat these infections?
There is a culprit here, so let’s take a closer look. Behind the misdiagnosis of hundreds of thousands (potentially millions) of people, are embedded chronic urinary tract infections that involve biofilms.
Biofilms And Persistent UTI

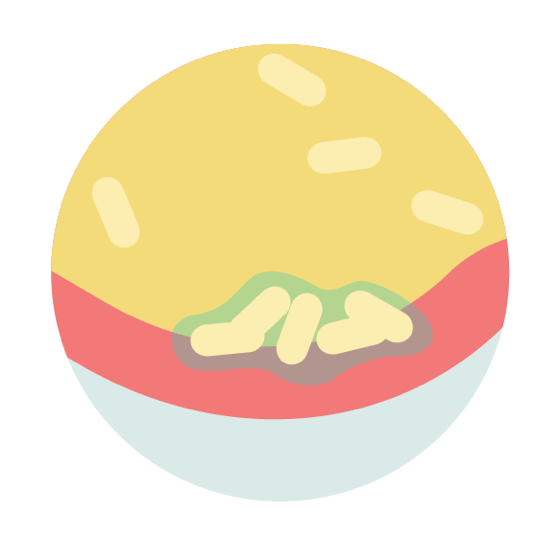
In the case of a chronic urinary tract infection, a biofilm is a community of bacterial cells that stick together and adhere to the bladder wall. These cells then produce a protective slime that shields the bacterial community from antibiotics and the natural defences of the body.
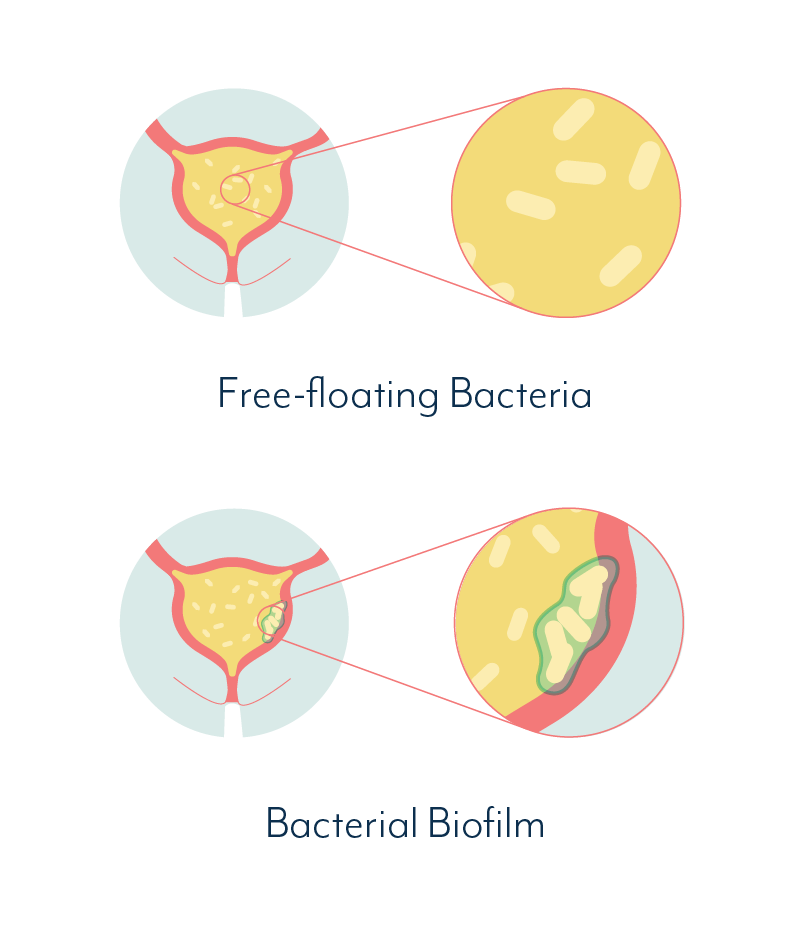
This goopy shield makes diagnosis and treatment very difficult. And while the bacteria are contained within their shield, the body is less likely to mount an effective response to their presence.
When bacteria are periodically released or escape from the biofilm, the body recognizes a threat. This triggers an inflammatory response, heightening symptoms of a UTI. This can be experienced as a cycle of acute symptoms, followed by periods of fewer or no symptoms.

“I get a UTI every month or so. In between each really bad UTI I would feel mostly better, but I’d often have sensations like another UTI was coming on. I was continually drinking water to try and prevent it, but, like clockwork, my symptoms would suddenly get much worse and I’d end up with another full blown UTI.”
We hear many people refer to this as a cycle of ‘flare ups’ or ‘episodes.’ This implies they believe it to be a continuous, chronic issue with both acute and symptom-free phases. Evidence shows they are probably right.
For those who suffer from a chronic urinary tract infection, the symptoms and ongoing pain can be debilitating, dramatically and adversely affecting their daily lives, as well as their overall mental and physical health.
How Biofilms Can Cause Your UTI Symptoms To Come And Go
Let’s compare the science of biofilms with the symptoms a sufferer of a chronic urinary tract infection may experience, using E.coli as an example pathogen:
 |
|
| Stage One | THE SCIENCE: • Infection and inflammation of urinary tract caused by invasion and multiplication of bacteria or other pathogen. HOW IT FEELS: • UTI symptoms, eg burning when urinating, urgency |
 |
|
| Stage Two | THE SCIENCE: • Free-floating bacteria form a weak attachment to the bladder wall • Antibiotics can still be effective during this stage HOW IT FEELS: • Without effective treatment, UTI symptoms remain as body continues to defend against the threat |
 |
|
| Stage Three | THE SCIENCE: • Bacteria establish a strong attachment to the bladder wall and a protective biofilm structure begins to form • Protection from antibiotics increases; treatment becomes more difficult HOW IT FEELS: • Without effective treatment, UTI symptoms remain as body defends against the threat |
 |
|
| Stage Four | THE SCIENCE: • Free-floating bacteria are flushed from bladder via treatment or natural body defenses • Biofilm remains intact HOW IT FEELS: • UTI symptoms decrease or disappear |
 |
|
| Stage Five | THE SCIENCE: • Biofilm community formation continues • Protection against antibiotics increases as the biofilm develops HOW IT FEELS: • No UTI symptoms, or low level chronic symptoms |
 |
|
| Stage Six | THE SCIENCE: • Biofilm detachment • Bacteria escape biofilm and enter urine as free-floating bacteria HOW IT FEELS: • ‘Recurrence’ of UTI • UTI symptoms return |
 |
|
| Stage Seven | THE SCIENCE: • New biofilm attachments may begin to form • Free-floating bacteria are flushed from bladder • Without appropriate treatment, the process repeats HOW IT FEELS: • A cycle of ‘recurrent’ UTI as the biofilm fluxes over time |
We should also note here that biofilms can be fungal as well as bacterial, and there may be more than one pathogen present in the bladder at any given time. In fact, biofilms can be complex and diverse communities of multiple pathogens.
 | “These organisms like to live in communities. Biofilms are like apartment buildings, and the longer that you've had this chronic infection, the more likely it is that you have more and more residents that have come to join the party. And they like to support one another, they live synergistically. It's sort of like a ball of yarn. You have to start pulling somewhere if we're ever going to unravel this big, knotted up mess.” |
For the sake of simplicity, and because bacterial infections of the urinary tract are much more common than fungal, we’ll stick to bacteria for our examples. But keep in mind, what causes a chronic urinary tract infection in one person is very likely different from the next person.
Bacterial biofilms can also be found INSIDE the cells of the bladder wall, forming intracellular bacterial communities (IBC). In fact, evidence of IBCs was found in about one fifth of urine samples from females with acute uncomplicated symptomatic UTIs.
Fascinated? A UK research team has put together a more in depth look at how biofilms and IBCs form for you to view.
Can You Test For Biofilms In The Bladder?
The presence of biofilms in the bladder is not far-fetched science.
The National Institutes of Health (NIH) estimates around 80% of all bacterial infections in humans involve biofilms.
Although the existence of biofilms in human infection has been accepted in medicine for decades, it is much more recently that attention has turned to their involvement in chronic UTI.
 | “In my opinion it's pretty clear that biofilms and IBCs are a true phenomenon, and it would explain why a given patient can get what seems like a perfectly appropriate antibiotic based on antibiotic susceptibility testing from cultured bacteria. Then as soon they stop taking the antibiotic, the same exact bacterial isolate comes roaring back with the same antibiotic susceptibility. Why wasn’t it wiped out? Well, I think sometimes it's IBCs, or biofilms. And then in other cases, it may be that they've reseeded themselves from their distal guts or their vagina as well." |
Traditionally, testing labs have focused on culturing and testing free-floating pathogens. If free-floating pathogens are identified, their susceptibility to antibiotics is also tested while they are in a free-floating state.
Once the susceptibility has been tested, it is possible to prescribe the right treatment.
The problem with these types of tests is that they do not specifically detect biofilm formations in the bladder. And therefore, they are not helpful in deciphering which treatments may be effective against microbes within a biofilm.
To figure out how to treat a chronic urinary tract infection that involves biofilms or IBCs, it would be necessary to test different treatments on any pathogens within a biofilm or IBC, rather than on free-floating, easy-to-target pathogens.
Newer UTI Testing Options
Some advancements in testing have been made. Researchers have been able to pinpoint indicators of biofilms and IBCs in the bladder. These include filamentous bacteria and exfoliated IBCs.
This isn’t as complicated as it sounds. All the first really means is bacteria that have taken on an elongated and/or branched shape as part of a bacterial community. Exfoliated IBCs refers to bladder lining cells that contain microbes and have been shed from the bladder into the urine. Both are signs of an embedded bladder infection.
Unfortunately, this area requires a lot more research. At the moment, tests to specifically identify an embedded chronic urinary tract infection are not available to the general public.
On a more positive note, there are tests available that are more accurate than standard culturing methods.
Tests that use DNA sequencing methods, like that offered by and MicroGenDX, have the ability to identify microorganisms in a urine sample, regardless of whether they are free-floating or were part of a biofilm.
You can read more about the issues with standard UTI tests, and how to find alternative UTI testing options in the next sections.
Treatment protocols for chronic urinary tract infection do exist, however, specialists who can administer these are few and far between. And this type of treatment requires regular monitoring to evaluate any improvement in the embedded infection.
Learn more about persistent UTI treatment approaches here.
Is Interstitial Cystitis Linked To Frequent UTIs?
We mentioned a study above, that found that 74% of survey respondents diagnosed with Interstitial Cystitis, had previously been diagnosed with recurrent UTI.
Research has also shown that a high percentage of females with Interstitial Cystitis may in fact have biofilms, IBCs, or both within their bladder, and that this is the cause of their ongoing infection and recurrent or continuous symptoms.
Interstitial Cystitis and associated conditions are considered to be incurable, however…
Interstitial Cystitis is a diagnosis of exclusion. This means IC is diagnosed in the absence of any other obvious cause. If a cause for your UTI symptoms is not identified by testing, a diagnosis of IC may be given.
Check out our expert video series to learn more about the chronic UTI and IC connection.
Reframing A Diagnosis Of Interstitial Cystitis
We shouldn’t think of IC as a specific condition, after all, those who have been diagnosed with it experience a vast range of different symptoms. And a cause for the onset of those symptoms has not been identified.
Instead, we should think of the term as a placeholder, while we wait for a specific cause to be identified.
A diagnosis of exclusion leaves a lot of room for misdiagnosis. Some researchers now believe the insensitivity of standard testing methods may have led to large numbers of unnecessary diagnoses of IC. Take a look at our interview with Dr. Roscoe Nelson, who discusses why accurate diagnosis is crucial.
 | "...if the [dipstick] test is negative, the sensitivity is such that there is no justification for claiming you do not have an infection... if the culture is negative it is again wrong to claim this proves an absence of infection; the culture is too insensitive. For these reasons, negative tests are unhelpful and a cause of terrible suffering." |
And this isn’t just theoretical. Hundreds of females previously diagnosed with Interstitial Cystitis – that is, the absence of infection – have been able to receive better testing that has identified an infection.
With an infection identified these individuals have gained long term treatment that relieves their painful symptoms and has often led to complete resolution of the issue.
 | “I am very careful about labelling patients with IC, I think a lot have occult UTI with difficult to culture organisms. By utilizing more accurate testing methods we are able to identify pathogens in many cases, and develop appropriate treatment.” |
When To See A Doctor For A Chronic Urinary Tract Infection
If you’ve had a UTI previously, you are in a much better position to recognize the symptoms, and you may feel confident in what action to take.
You may even be able to take this action at the first sign of a UTI, and prevent the symptoms from escalating. This doesn’t necessarily mean you have cleared the infection. If you’ve read the fascinating tale above about chronic urinary tract infection and biofilms, you’ve probably realized that by now.
For females with a chronic urinary tract infection, it’s not just about treating isolated symptoms, it’s about breaking the cycle and eradicating the underlying cause.
How UTI Treatment Should Look
The ideal scenario wouldn’t involve a UTI at all, we get that. But once you’re on that roller coaster, you really need to find a way off safely. This is what the ride should look like…
Symptoms → Test → Results → Diagnosis → Treatment → Cure
Anyone who has experienced a chronic urinary tract infection can tell you this isn’t always how it pans out.
Instead, for many females, parts of the sequence are missing, and a cure has been out of reach. There are a number of reasons for this, which we’ve covered in our article on UTI testing, so we encourage you to read that next.
Getting tested to discover the cause of your UTI symptoms is the best path to a permanent solution.
You should get tested if you:
- Have had more than 2 UTIs in the last 6 months, or more than 3 UTIs in the last 12 months.
- Have continuous or ongoing UTI symptoms, but haven’t received a diagnosis.
- Are uncomfortable taking antibiotics without knowing what exactly you are treating.
- Have recurrent UTIs and have never been tested.
And the best way to get tested is to see a doctor. Finding the right doctor, however, can also be tough. But first things first.
Now that we’ve convinced you to pursue testing, we need to tell you something…
Getting accurate testing for UTIs is extremely difficult.
So in the next article we’ll share some frustrating facts on why this is, and provide a few tips on how to get better UTI testing. It’s always best to arm yourself with information before embarking on a journey towards better health, and you’re in the right place.
Share your questions and comments below, or get in touch with our team. To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page.

I’ve been suffering with constant uti with years and no one seems can help me I had the camera in my bladder didn’t show anything ..blood and infection show up all the on the dip sticks in Dr surgery but she sends them away to grow but it doesn’t grow anything ..I am sick with a lot of them with temp and end up in bed ..I not able to plan anything in case I get sick ..even work is suffering ..the antibiotic helps but doesn’t take it away can anybody help me ..I’ve tried everything
Author
Hi Eileen, I can understand your frustration. An explanation for your negative urine culture tests could be contained in our article about why that happens more than it should (there’s a good chance the test is just wrong). If you’d like to send me a direct message and let me know where you’re based, I may be able to share details of chronic UTI experts that might be helpful. Melissa
Hi
I’ve always had UTI’s here and there my entire life, but I know to do my best to flush my system and the symptoms will go away on their own.
A month and a half ago I started taking Topamax as an anti-seizure medication and I have had UTI symptoms pretty much non-stop since then. Once I think I’ve kicked the issue, the symptoms return with a vengeance. When I brought this up to my neurologist, she told me to take antibiotics to get rid of the infection since my records show I’m susceptible to UTI’s… I feel helpless and like that’s not the answer, as I’m not a huge fan of taking antibiotics.
Is it possible I’m not crazy and the medication is somehow to blame for this?? I’m currently weighing my options to rid the issue.
Thanks in advance for any advice.
Author
Hi Tina, we hear from a number of people whose symptoms change (for better or worse) with different medications but it’s impossible to comment on any specific one. If you like, you can send me a message with more info about your experience and perhaps I can share some useful resources about different approaches. Melissa
Hi
I’m 71 have repeated Kidney infections for the last 3 years.
Every 2 months.taking long term antibiotic still get infections.
Can anybody help
Thanks
I feel so upset and down now
I’ve seen urologist and GP
Author
Hi Ursula, sorry to hear you’re experiencing that, you’re definitely not alone. Are you able to send me direct message and let me know where you’re located so I can share further resources? Melissa
Hi there. I’m a 52 year old female and am on my 4th UTI in 7 months. Prior to this, I had only one UTI in my life. I recently saw a Urologist who performed a Cystoscopy and said everything looked fine with my bladder but is sending me for a scan on my kidneys. He did mention that some women do experience an increase in UTIs at Menopause so I’m not sure if that’s the culprit. I’m concerned about constantly having to take antibiotics and don’t know how much longer I can deal with the pain and burning. 🙁 Any suggestions on next steps? Thank you!
Author
Hi Mary, I can send you some studies about the increased risk of UTI after menopause, and the ways that treatment may differ, if you’d like to read them. If so, you can send me a direct message so I can share via email. Melissa
Hello I am a 35 yr old female and have always had uti’s but here in the last year they have gotten worse. It seems like everytime after intercourse I seem to get symptoms or a full blown uti if I dont take Uristat to calm my bladder. I seem to get them every week and have symptoms every week and some weeks more severe than others. I drink mostly Gatorade and just a little bit of sweet tea. I flush my system as best as I can when I feel symptoms coming on and sometimes it seems to work other times it does not and I have to go and get antibiotics but they will give me antibiotics before they truly know if it is positive or negative. Most of the time they are negative and they can’t tell me why.
Any suggestions that might help?
Author
Hi Gena, we have some information on why tests can be negative despite your symptoms, and other types of testing you can try. If you have any questions about these, feel free to contact me. Melissa
hi im 25 years old ive been struggling with recurring infections for two years , my gp has tried all kinds of antibiotics they dont always work , iv been to a gynae that told me i have mild pcos and that i should lay off the antibiotics , but every month after my period i start getting a yellow discharge with bad lower back and dont know what to do
Author
Hi Noorani, can you get in touch with a little more info so I can share resources that might be useful? Melissa
Hi I’m 22 years old and for years I’ve had utis back to back. I get one then go to the er in so much pain. I’d finish my antibiotics and I’ll be okay for a few days then I’ll get another one. Some doctors are shocked when I’ve came in and had one so bad that they couldn’t believe I wasn’t feverish…. I just have birth 3 months ago and during the whole pregnancy Ive only haved 1 but now it’s starting again. This is definitely not what I want to deal with for the rest of my life. Having them every week or 2 will drive someone crazy. Doctors can’t seem to figure it out. Everything looks normal to them
Author
Hi Cheyanne, you’re not alone in this experience. So many people have ended up in a cycle of chronic UTI, many of them because of inaccurate testing. You may need to pursue alternatives such as advanced testing, or working with a chronic UTI specialist. I saw you sent me an email so I’ll send more info there. Melissa
I can relate to what everyone has written.
I can’t remember how long I have had this problem?? More than TEN years for sure.!!!
What can we do?
I’m ready to fight!! This is awful that so many women have been suffering.
Keep me posted. God help us!!
Sincerely, Dolly Carnine
Author
Hi Dolly, it certainly takes a lot of fight to advocate for yourself and find answers! I saw you emailed me, so I’ve replied with some more info there. Melissa
hi there, I’m a 32 year old female. When I met my husband 5 years ago, I started getting UTI’s more frequently. I went to a few urologists and they recommended taking an antibiotic every time we had sex. I wasn’t super comfortable with it, but just wanted the cycle to stop. And it did help! But overall, I didn’t like that I was taking antibiotics so frequently, so I stopped. Since December, I have had (pretty much) non stop issues. Sometimes, full blown painful UTI’s, but mostly small amounts of discomfort here and there. At the beginning of the year I had a cystoscopy, and the doctor said everything looked normal anatomically and inside my bladder. I really don’t want to keep turning to antibiotics.
Author
Hi Andi, we have some info on why the use of prophylactic antibiotics is questionable, so you’re not alone in your concern there. We’re working on some new content about UTIs related to sex, but in the meantime, if you send me a message I can share more there. You also might like to read more about advanced testing and treatment. Melissa
Does Uqora help? I have heard good things about this product?
Author
Hi Angela, we don’t recommend specific products on our site. For any product, it’s best to research the individual ingredients, and look to see if the product has been tested in any studies before making a decision whether to try it. If it helps, we have some information about popular home remedies, with links to studies where they are available. Melissa
Hello! I am a 31 y/o female. I’ve suffered from chronic UTI since 2011. It has taken such a huge toll on my quality of life. I’ve started a regimen of probiotics, regular d-mannose intake, and NAC daily. Regarding the NAC – it appears that this potentially makes UTI symptoms worse before they get better. I am accurate in saying/thinking that? I’ve noticed over the past 2 weeks since the NAC kicked in that the symptoms pop up every 2 days or so. This is without having sex or doing anything else that typically causes me to have symptoms. I am hoping the d-mannose helps to pull all of the broken bacteria out… but just curious if the NAC breaking down the biofilms could be causing me to have the recurring symptoms every few days right now. Thoughts? Any help is greatly appreciated!
Author
Hi Lauren, although biofilm dissolvers are becoming more widely used, there are still no studies that look at whether they reach the bladder or are effective there. Anecdotal evidence from other users suggests that they can cause flare ups of symptoms, but we can’t confirm one way or another until those studies are done! D-mannose has only been shown to have any effect on E. coli, so whether it works may depend on what’s causing your infection. You can send me a message directly if you have other questions. Melissa
I have occasional flare-ups of UT inflammation – usually testing with no infection – which are apparently related to prostate problems – still waiting for my next appt with the urologist. Every single time I take a regular dose of NAC, my upper UT (prostate area) will be “on fire” within the day, as if scalded. NAC is extremely acidic – likely much more than ascorbic acid, which never causes this “scalded” feeling.