Interstitial Cystitis Treatment With Ruth Kriz
There are very few practitioners achieving Interstitial Cystitis treatment success. Ruth Kriz is one of them.
Ruth Kriz, Nurse Practitioner, has been treating patients with chronic urinary issues for 35 years. Her interest in chronic UTI and Interstitial Cystitis (IC) stems from personal experience.
We get a lot of questions about Ruth Kriz’s approach to recurrent UTI and Interstitial Cystitis treatment, so we had a good long chat with her, and spoke to a number of her patients. Below we’ve shared what we learned.
Jump To Section:
- Ruth’s personal battle with Interstitial Cystitis >>>>
- The chronic infection and Interstitial Cystitis link >>>>
- Ruth’s approach to chronic UTI and IC testing >>>>
- Ruth’s chronic UTI and Interstitial Cystitis treatment approach >>>>
- Can you treat an antibiotic resistant bladder infection? >>>>
- Interstitial Cystitis treatment success >>>>
Ruth’s Personal Battle With Interstitial Cystitis
Although Ruth’s experience with Interstitial Cystitis was over 35 years ago, little has changed in the journey to diagnosis.
 | “Like with most people, when you personally experience the problem, you have a whole new motivation to figure it out. I developed Interstitial Cystitis and my first urinary tract infection in my early 30s, and went the traditional route urine culturing and antibiotics, and basically was failed by the medical profession.” |
After developing urinary tract symptoms in her early 30s, Ruth went through multiple rounds of urine culture tests and antibiotics.
Eventually, after a number of negative urine cultures, Ruth was told she did not have an infection despite her ongoing symptoms. She was left with a diagnosis of Interstitial Cystitis, and was given no further assistance by the medical profession. Interstitial Cystitis treatment was virtually unheard of; management of symptoms was the only option.
As a Nurse Practitioner herself, Ruth was fortunate to be connected to researchers working on different culturing techniques. With their help she was able to begin identifying infections in her own bladder, and start treating them.
This Interstitial Cystitis treatment approach worked so well for Ruth, she hasn’t experienced any urinary tract infections for the last 25 years. She made it her life’s work to help other people with similar issues, who weren’t being helped by traditional medical approaches.
 | “I was told my urine culture was negative, and I therefore didn’t have an infection. I was subsequently diagnosed with IC, but occasionally, during a symptoms flare, I would be culture positive. Eventually I pursued better testing, and found I’d probably had an infection the whole time. I’m slowly recovering, with treatment, and I’m glad I didn’t accept my diagnosis in the end.” |
The Chronic Infection And Interstitial Cystitis Link
Interstitial Cystitis is a diagnosis of exclusion, and it’s not new. There are records of IC from the 1800s, before antibiotics existed.
You can be given the label of IC once enough other potential issues have been ruled out. This has also come to mean that infection must be ruled out using a standard urine culture.
The problem is that we now know that standard urine culturing techniques are significantly inaccurate. In fact, in up to 50% of tests, the results are wrong.
This has left countless UTI sufferers with false negatives and incorrect findings, leading to incorrect treatment or no treatment at all. You can read about Emma’s experience with a misdiagnosis of IC and how she learned of the root cause for her symptoms.
 | “IC became a diagnosis of exclusion - they ruled out bladder cancer, an obstruction or some functional problem, and if you were culture negative, then you had this bizarre unknown condition called Interstitial Cystitis. So the line became very fuzzy between chronic urinary tract infections and Interstitial Cystitis.” |
Fortunately, science has provided new ways to look at chronic urinary tract conditions. In the case of Interstitial Cystitis, where standard urine culturing has been unable to pinpoint the cause, DNA sequencing has identified infection in thousands of IC patients.
In fact, Ruth has discovered infection in a high percentage of her IC patients. This means for the first time for many, there are chronic UTI and Interstitial Cystitis treatment options, and a chance at recovery.
 | “When I first started getting my urine tested after 11 years of chronic urinary tract symptoms and six years of chronic pain, first, I prayed they wouldn't find anything. And then I started praying they would, because I knew that if you find something you can treat it and that gives you hope.” |
If you’ve been diagnosed with IC after previous negative urine culture tests, you may now have an opportunity to reassess your diagnosis.
How Urinary Tract Infections Can Develop Into IC
One study found that 74% of females diagnosed with Interstitial Cystitis had previously been diagnosed with recurrent UTIs.
 | “I would get a UTI, take the antibiotics and the symptoms would disappear, then suddenly, weeks or months later I’d have another UTI. So I’d take the antibiotics and the symptoms would disappear… Rinse and repeat basically. The symptoms would always come back and eventually I was diagnosed with IC.” |
So what exactly is going on inside your bladder? Why don’t the UTI antibiotics work and why can recurrent UTIs result in a diagnosis of IC?
There is a potential culprit here, so let’s take a closer look.
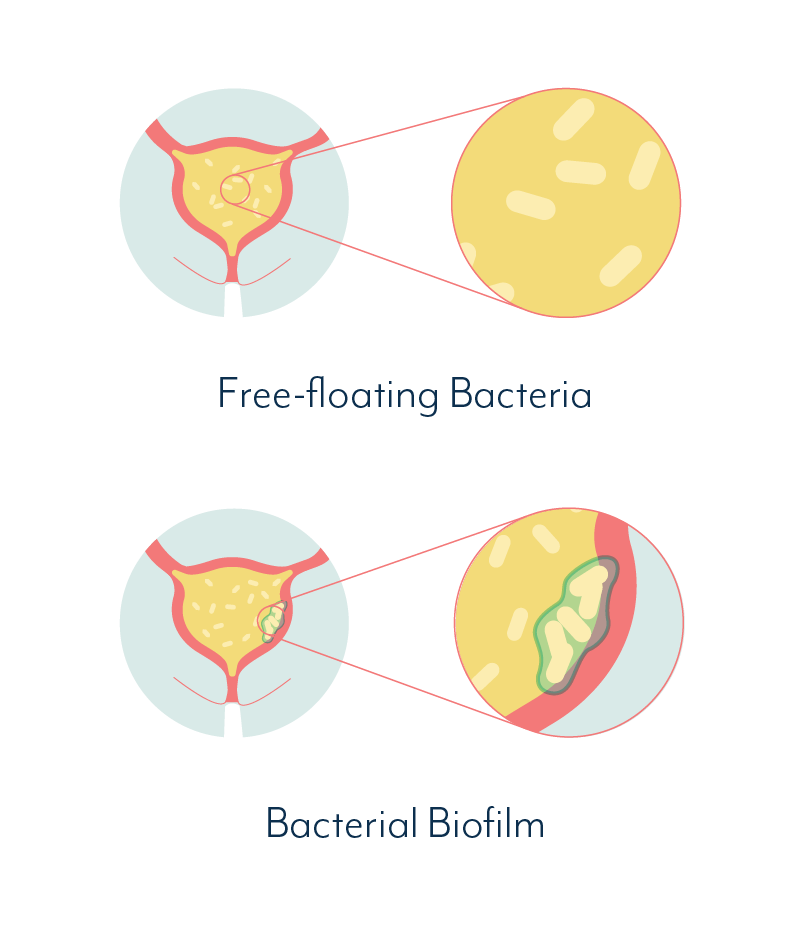
Chronic, Embedded Infection
It’s quite possible that what you have considered to be separate UTIs or IC, is actually caused by an infection embedded in your bladder wall, that never completely goes away.
The symptoms may come and go, or maybe you’ve reached the point where you have symptoms 24 hours a day. It’s different for everyone.
A chronic, embedded infection like this is caused by a biofilm and/or by pathogens living within your bladder wall.
 | In the case of a chronic urinary tract infection, a biofilm is a community of bacterial cells that stick together and adhere to the bladder wall. These cells then produce a protective slime that shields the bacterial community from antibiotics and the natural defences of the body. |
Your body naturally flushes out free-floating pathogens in your urine, but biofilms and pathogens within the bladder wall remain intact…
Biofilms and intracellular communities make diagnosis and treatment very difficult.
When the body recognizes a biofilm or intracellular community as a threat, it may begin to slough off pieces of the bladder wall, in an attempt to rid the bladder of these persistent pathogens.
Many people describe seeing what appears to be tiny, tissue paper like pieces in their urine. It’s likely these are actually tiny pieces of your bladder wall. This can be a good sign, as it means your body is trying to eliminate the infection.
 | “Sometimes I see these wispy white bits floating in the toilet after I pee. It’s usually when my symptoms are at their worst. I never understood why it seemed like parts of my urinary tract were coming out in my urine, but now it makes sense.” |
You may experience the biofilm phenomenon as a cycle of acute symptoms, followed by periods of fewer or no symptoms.
This is because bacteria or other pathogens are periodically released or escape from the biofilm, causing an inflammatory response which heightens the symptoms of a UTI.
For IC sufferers, these periods may be experienced as flare ups, or it may feel as though you suddenly have a ‘real UTI on top of your IC.’
If your symptoms are actually caused by a chronic infection, you may have an opportunity to pursue Interstitial Cystitis treatment, rather than symptoms management alone.
Can You Test For Biofilms Or Chronic Infection?
While a biofilm remains intact, it may be difficult to identify its presence. If it ruptures, or the body sloughs off its own bladder wall cells, pieces of the biofilm may be shed into the urine.
Importantly, standard urine culture is unlikely to identify pathogens contained within a biofilm, even when pieces of it are within your sample. Culturing relies on being able to quickly grow bacteria, and bacteria within a biofilm are not usually in a growth phase.
DNA sequencing methods, like those Ruth utilizes, can identify pathogens within a biofilm in a urine sample. This is because they do not rely on bacterial growth. Instead, they compare all DNA found against a database of microorganisms.
By using these methods, Ruth is able to more accurately map out a comprehensive approach to Interstitial Cystitis treatment.
 | “These organisms like to live in communities. Biofilms are like apartment buildings, and the longer that you've had this chronic infection, the more likely it is that you have more and more residents that have come to join the party. And they like to support one another, they live synergistically. It's sort of like a ball of yarn. You have to start pulling somewhere if we're ever going to unravel this big, knotted up mess.” |
Ruth’s Approach To Chronic UTI And IC Testing
Up until about 3 years ago, Ruth used a soy broth culture technique that had the ability to identify many infections that were missed by standard urine culturing.
As science caught up, DNA sequencing methods became more widely available. Ruth currently uses different types of DNA sequencing – polymicrobial antibiotic susceptibility testing by Pathnostics, and Next Generation Sequencing by MicroGenDX.
DNA sequencing has the ability to identify known pathogens, without relying on flawed culturing methods. The results Ruth achieved with these techniques showed that even the broth culturing method was missing infections.
With the help of DNA sequencing, Ruth now finds most of her chronic UTI and IC patients not only have multiple bacterial infections; around 15% also have fungal infections in the urinary tract.
 | “In the four years that I have been doing the DNA testing of urine, I have found infection 100% of the time in my patients that have been diagnosed with Interstitial Cystitis. I don't have a single person who has an IC diagnosis that we haven't found infection.” |
This is particularly interesting for those with an IC diagnosis based on a negative standard urine culture.
Many people report a negative culture despite symptoms such as pain, urgency, frequency, burning, and tissue paper-like bladder lining cells in their urine.
 | “There’s an old expression, if it looks like a duck, walks like a duck, and quacks like a duck. It's gotta be a duck. And so to have somebody who has pain, urgency, frequency and burning, and yet they're told they don't have an infection because a urine culture was negative, who do you believe? Are you treating a lab result? Or are you treating a person?” |
Technology has advanced in such a way that a true diagnosis and successful Interstitial Cystitis treatment may now be possible for many.
How To Collect A Urine Sample For Advanced Testing
In order to develop the right Interstitial Cystitis treatment approach, it’s important to find out as much as possible about what’s happening in the bladder. This includes collecting a useful urine sample.
Studies have shown that it is very difficult, if not impossible, to collect a sample that does not contain contamination from the surrounding skin, without the use of a catheter or other invasive methods. This isn’t always accessible, nor desired, so we’ve provided some tips on how to collect a urine sample for various types of testing. Ruth has her own advice to add to this.
How diluted or concentrated your sample is can impact the accuracy of your results. So Ruth recommends the following:
1. Urinate without collecting a sample, and try to stop and start the stream repeatedly, in order to flush any contaminants out of the urethra.
2. Wait 1-2 hours, and in this time, don’t drink a lot of fluids.
3. Wash the area around the urethra with plain soap and water. Don’t use antibacterial or alcohol wipes. This may wash chemicals into your sample that can kill the bacteria you’re trying to find.
4. Collect a midstream urine sample, at a volume according to the instructions included in the kit.
If you’re really symptomatic and need to urinate more frequently than every two hours, scratch the preparation pee. You can just start at step three.
As a general tip – and this applies to every female – Ruth recommends urinating every three hours when you’re awake. That’s about how long it takes bacteria to ascend and begin colonizing the urethra.
Ruth Kriz’s Chronic UTI And Interstitial Cystitis Treatment Approach
Ruth has achieved an Interstitial Cystitis treatment success rate of around 80%, which is in line with the small handful of other chronic UTI specialists around the world.
Chronic UTI and Interstitial Cystitis treatment can take a long time, and it’s likely that the longer the problem has perpetuated, the more aspects of health will need support.
 | “My first goal for each patient is to get them out of pain, but instead of just managing the pain, I like to discover what the root causes are and address those. At the end of the day, if all you're doing is managing symptoms, you’re never going to get people well. The information from MicroGenDX, and Pathnostics tests tell me what the underlying problems are, so I can help address them.” |
Ruth’s typical Interstitial Cystitis treatment approach is to use oral antibiotics or oral antifungals first. She finds this works well for many people.
Certain patients may choose to use bladder instillations, particularly when infections have become deeply embedded in the bladder. This may also be preferred by those who experience issues related to oral antibiotic use (antibiotic resistant pathogens, deteriorated gut health etc).
In this case, Ruth is able to work with a compounding pharmacist to develop an exact formula for direct instillation into the bladder via a catheter. The instillation may contain antibiotics and/or antifungals, often combined with a biofilm dissolver.
Biofilm Dissolvers
The biofilm dissolvers Ruth recommends contain enzymes that break down biofilms. They also help to remove any heavy metals that may be strengthening the biofilm structure. In essence, this causes the biofilm to begin to collapse as it loses its structural integrity.
We should note here that as yet, there are no studies that test the effectiveness of biofilm dissolvers within the bladder. The effect of specific compounds has been demonstrated in other uses, and outside the body.
Patients who use biofilm dissolvers sometimes report a flare up of symptoms which may be an indication that it is working as intended.
Where To Buy Chronic UTI Products
As Ruth winds up her practice, she has been implementing a number of things to pass on her knowledge. First, she’ll be training other practitioners in her approach.
Second, we have been working with Ruth to ensure the products she recommends for different patients are available online. We’ve launched an online store dedicated to female urogenital health and created a collection of the UTI prevention products Ruth recommends.
Bladder Instillations
Bladder instillations are administered by the patients themselves, using a very small, pre-lubricated, pediatric catheter, usually twice per day for two weeks.
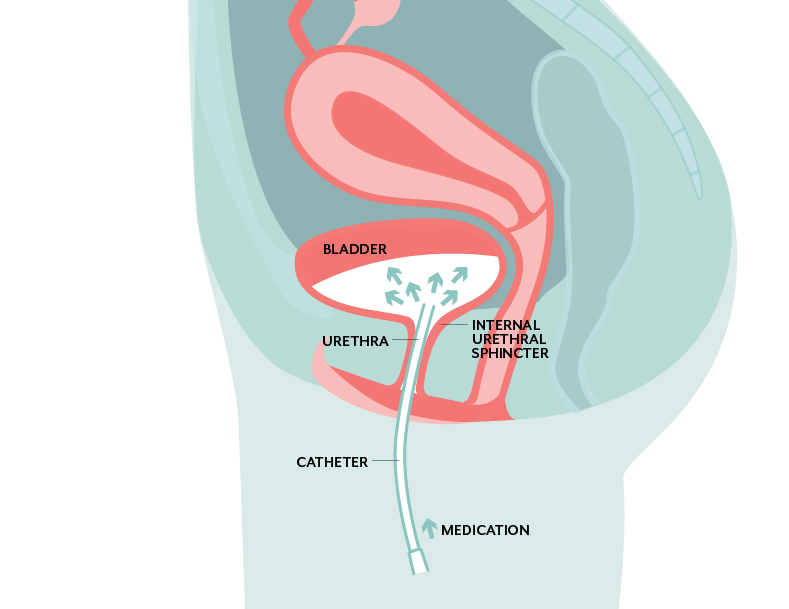
Medication is placed into the catheter, which is then inserted through the urethra. The medication is instilled into the bladder, and ‘held in’ for as long as possible. Many people hold it overnight.
Download Ruth’s explanation on bladder instillations as a treatment option for chronic UTI, if you’d like to share this with your own practitioner.
 | “Because we're able to combine medications with enzymes that break down biofilms, and deliver these directly to the bladder, this is probably the most exciting treatment tool I've had in decades. It gets to where the infection is. It penetrates the deepest, and people who use instillations tend to make the most progress in the shortest amount of time.” |
Interstitial Cystitis Treatment When Biofilms Are Involved
 | “We know that certain people genetically do a better job of making biofilms than other people, certain people have more difficulty breaking those biofilms down because of their genetics. We also find with biofilms, that once you treat the tip of the iceberg, there's a whole set of other problems underneath. We find multiple pathogens in these biofilm communities.” |
Whether you choose antibiotic bladder instillations or oral antibiotics, Ruth recommends repeat testing at different stages of chronic UTI and Interstitial Cystitis treatment. This ensures the treatment is still correct for any pathogens identified.
Why?
As one layer of the biofilm is broken down, you may find different microorganisms underneath. If so, the treatment approach may need to be changed accordingly.
 | “I took oral antibiotics for two weeks, then tested again. The results showed a different set of possible pathogens, so Ruth changed the treatment and I took another two week course. The third test again showed changes in organisms in my bladder so we shifted treatment to match. With each round of treatment, my symptoms improved.” |
While long term antibiotics may chip away at a biofilm and result in successful treatment over time, Ruth has found that biofilm dissolvers can speed up the treatment process by exposing infections that may be buried.
 | “Organisms within a biofilm will competitively inhibit each other. When you repeat the testing, almost 100% of the time, we find additional infection than we did on the initial test, because we are breaking down these biofilms.” |
Because newer testing methods are able to identify microorganisms that are difficult to culture; things that have never before been identified in the urinary tract are appearing in DNA test results.
Newly discovered urinary pathogens can mean a new treatment approach is needed, and this often requires in-depth research. Ruth works with a compounding pharmacist to develop custom treatment combinations when required.
Can Hunner’s Ulcers Heal?
Ruth believes that as with ulcers elsewhere in or on the body, it is possible for the body to heal Hunner’s ulcers on its own. Ruth likens Hunner’s ulcers in the bladder to stomach ulcers.
Thanks to scientific research, we now know that a certain bacterium called H. pylori causes a significant portion of stomach ulcers, and that when the infection is properly treated, the ulcers can heal.
In this same way, Ruth has seen many patients whose Hunner’s ulcers have healed once the infection in the bladder was effectively treated. For a few patients, this recovery has been documented by follow up cystoscopy. For others, the resolution of their symptoms has been the strongest indicator.
An Integrative Approach To Interstitial Cystitis Treatment
When it comes to healing a urinary tract that has been tortured for years, it’s not just about finding the bugs causing the infection and killing them. It’s also about ensuring your body and your immune system can repair and recover.
 | “I recently read a book on Alzheimer’s which used the analogy of there being 36 holes in your roof to illustrate multifactorial issues in chronic illness. It’s not enough to patch one hole - you’ll still get rain coming in. I feel it's the same way with chronic UTI and IC. People have infections that have become chronic because their body's own immune system can no longer do the work it's supposed to do and we have to find out why.” |
The analogy of 36 holes in the roof can apply to chronic UTI and IC sufferers. In Ruth’s opinion, most people with chronic UTI or IC are likely to have at least 5 or 6 additional issues to address.
It may seem complicated and as though there are many pieces to the puzzle, but recovery is not insurmountable.
Ruth looks in detail at every individual’s medical history and symptoms. She then recommends a series of tests that help identify which ‘holes’ they’re dealing with. Then it’s a matter of prioritizing issues for treatment.
The Immune System And Chronic UTI
Chronic illness of any kind can depress the immune system. If you’ve suffered from chronic UTI or IC, your immune system has taken a hit. On top of bladder issues, infection elsewhere in the body may be contributing to your body’s inability to heal.
Because of this, Ruth looks for other infections, particularly tick-borne infections and certain viruses. She finds that around 90% of her patients have a co-infection of some type.
Other issues that may impact the immune system include exposure to heavy metals or mold toxins, chronic pain, adrenal stress and thyroid function.
It may be necessary to first address other elements impacting your immune system, in order to overcome chronic bladder infection.
Sex And Chronic UTI
While most practitioners do not consider the potential involvement of a sexual partner in cases of chronic UTI, there is evidence that they should.
If you feel better after UTI treatment, but then find that your UTI symptoms flare up 24 to 48 hours after sex, it’s possible you are being reinfected by your partner.
One of the reasons it’s difficult to pinpoint where the infection is coming from, is that males can often carry bacteria without experiencing symptoms (asymptomatic). They may feel completely fine, while you do not.
Testing for infectious load in males can require testing the semen in addition to, or instead of the urine. This is because bacteria may be originating from the prostate rather than the bladder.
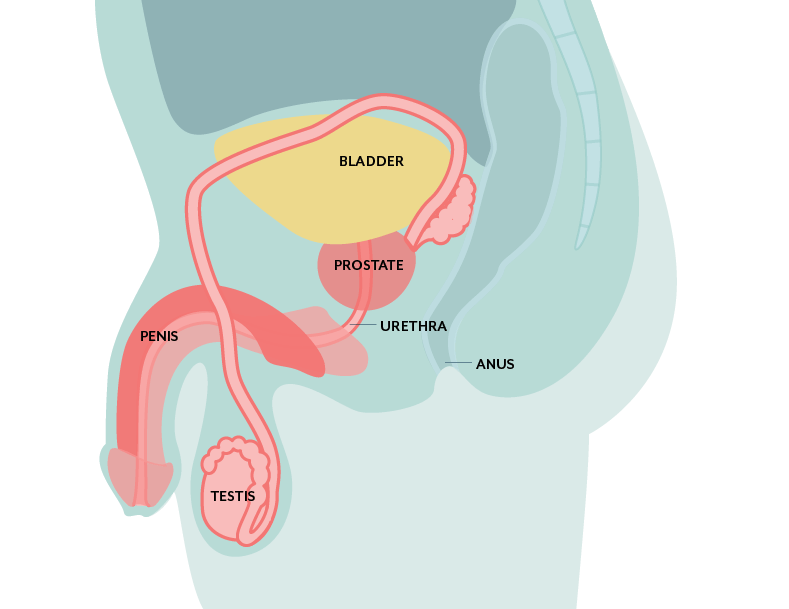
Treatment of prostatitis (prostate infection) is more complicated than treatment of cystitis (bladder infection) because the prostate gland is encapsulated. There is a limited number of antibiotics that penetrate the prostate and treatment typically takes longer as a result.
If you think your chronic UTIs may be related to sex, it’s a good idea to speak with your partner and your doctor about it.
Learn more about UTI and prostatitis diagnostic methods in our video expert series.
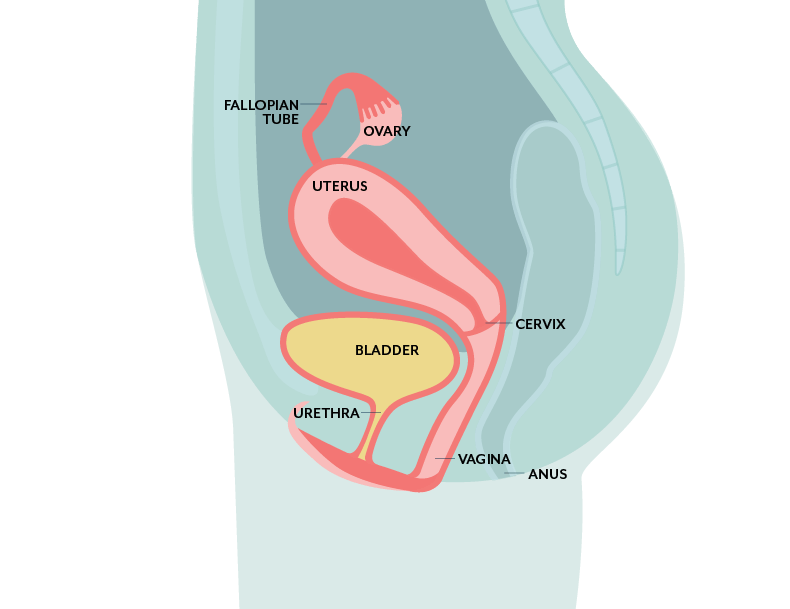
Vaginal Health And Chronic UTI
The urethra and the vagina are in pretty close proximity. It should come as no surprise that the health of one is closely linked to the health of the other.
Recent research by scientists at Loyola University has demonstrated that the urinary and vaginal microbiomes share many of the same microorganisms.
A dysbiosis in the vaginal microbiome can continuously seed pathogens into the urinary tract, causing infection. A dysbiosis refers to bacteria and fungi that are not supposed to be in the vagina (or at least not at certain levels) but are.
In postmenopausal females this can become even more prevalent. This is because the vaginal environment becomes less healthy for the good, healthy bacteria that should be living there.
These infections are generally assumed to be caused by Candida albicans (yeast) or Gardnerella (Bacterial vaginosis or BV). However, researchers have found much more varied microorganisms that may be causing infection.
In her own work, Ruth has found people to be colonized vaginally with Enterococcus, E. coli, and Klebsiella, to name a few. Test results also often confirm identical pathogens in both the urinary tract and the vagina.
Where chronic BV is an issue, Ruth will often recommend antibiotic suppositories or gels. These are compounded according to the specific bacteria found. This targeted approach has higher success than the broad spectrum antibiotics that are typically utilized.
Can You Treat An Antibiotic Resistant Bladder Infection?
This is a question that comes up a lot: Is it possible to treat an antibiotic resistant infection?
It’s important first to understand a few things:
- Antibiotic resistance means that a specific pathogen is resistant to specific antibiotics. It does not mean that your body is resistant to those antibiotics or that you cannot take them. (Fungi can also become resistant to antifungals).
- Resistance can mean a pathogen is able to defend itself against a specific medication. It does not necessarily mean that drug cannot treat the pathogen given enough time.
- A pathogen may be resistant to some drugs, but not others. So resistance does not always mean there are no options available.
One of the ways Ruth has been able to get around antibiotic resistant infections is by utilizing bladder instillations, as mentioned above.
Because instillations are not taken orally, it is possible to use a range of antibiotics that are typically only delivered by IV (directly into the veins). This effectively targets microorganisms in the bladder that have not been exposed to these antibiotics previously.
This could mean that IC or chronic UTI sufferers who have not taken antibiotics for years may now have treatment options available to them.
Interstitial Cystitis Treatment Success
Ruth estimates a success rate in her Interstitial Cystitis treatment approach of over 80%. Given a chronic bladder infection can be around for a long time, decades for some people, it can also be a long road to recovery.
 | “I will say that the people who stay with the process, even though it takes a lot of self discipline, and who are committed to getting their lives back, do the best. I think what sometimes happens is - I get them out of pain with their bladder, but if they don’t complete the healing process, other factors can cause them to lose their healthy status down the road.” |
Part of how well and how quickly you can recover comes down to how seriously you commit to the process of getting better.
Big changes may be necessary for some people. And while testing for unknown factors can be scary, if you don’t start the process and see it through, you may never be well.
If treatment success rates are so high, why is it so difficult to find IC success stories?
 | “The psychology of this is very interesting. I know that when my own bladder got better, I got my healing and I ran. I intentionally got my life back and had some years that were completely normal raising my children, and I didn't want to revisit that part of my life that had been so dreadful. Once people have recovered they leave the IC groups and forums. Instead, they’re out there living normal, healthy, productive lives - working again, having children. It’s not surprising they want to put their IC behind them. I wish them well.” |
Ruth’s goal is to help people get totally healthy again; to get their lives back. What happens after that is up to the individual.
People don’t tend to hang around in forums and facebook groups once they are well. So don’t let online conversations discourage you from seeking better answers for yourself.
Prepare For An Appointment With An Integrative Practitioner
An integrative approach means the practitioner will consider additional factors beyond your bladder.
You may be asked detailed questions about not only your own medical history but that of your immediate family. These questions are looking for genetic factors that may impact your body’s ability to heal. To help with this process, we’ve provided some tips below.
1. Ask parents or surviving relatives about your family history. This includes heart attacks, strokes, high blood pressure and anything else worth noting.
In many cases a bladder infection is not the only issue that needs to be addressed to get your immune system back on track. Symptoms you may consider insignificant may be part of the key to getting well.
2. Track your symptoms; headaches, cognitive issues, sleep issues, gut issues, joint pain etc. Anything that ails you may be relevant.
Ruth finds tick-borne infection is a factor in around 75% of her patients. She has also identified a number of other attributes that are shared among her patients, such as exposure to mold toxins, breast implants and other genetic factors. It’s a good idea to discuss what additional information may be useful, with your own practitioner.
What Types Of Patients Can Benefit From Ruth’s Approach?
Ruth specializes in Interstitial Cystitis (IC) and chronic urinary tract issues, but also sees patients with Lyme and other tick-borne diseases. About 90% of her patients are female, and a number of her male patients are partners of her female patients.
In most cases her male patients are asymptomatic despite their semen showing infection in tests. See the section above on sex and chronic UTIs for detail on what this means.
Can Your Own Doctor Work With Ruth?
Ruth has patients in 48 US states and 30 countries, and her waiting list is up to six months long.
Ruth is happy to work with any practitioner who is open to her approach. If you have a practitioner you wish to continue with, you may like to discuss this option with them.
After decades in practice, Ruth has started work on educational resources to help other practitioners learn about the intricacies of chronic bladder infection. She aims to support others in finding better ways to help their own patients.
 | “If a practitioner sees how frustrating it has been for their patient, and want to help but have been unable to, I think their heart is in the right place. They want to be genuinely helpful to this patient, but it's a little overwhelming to get into the details of how much work is involved in doing all the testing that’s needed. My great desire would be to not have my secrets die with me.” |
If you’re a practitioner and would like to learn more, you can get in touch with us or reach out to Ruth directly through her website.
To get answers to commonly asked questions about chronic and recurrent UTI, visit our FAQ page. Share your questions and comments below, or get in touch with our team.

Hi there, I was diagnosed with IC about 2 years ago and I’m still struggling with my symptoms. Thank you so much for this article, it really got me thinking. Is there someone near Tampa, Florida that may be able to help me? Thank you.
Author
Hi Jamie, I just sent you some more information on this by email. I hope it helps. Melissa
Hi there, I’ve been suffering from a diagnosis of moderate IC for the past 5 years that stemmed from a bout of recurrent UTIs from sex. Within the past year my symptoms have flared and I am getting a UTI almost every time I have sex. I was also diagnosed with a hypertonic pelvic floor and was in physical therapy for this over a year ago. I would like to see a doctor that you recommend in NYC/Brooklyn area , or please provide more information about getting on the wait list to see Ruth. Thank you
Author
Hi Tiffany, we sent you a few emails with different information that may be helpful. Melissa
Hi,
I am looking for a doctor in Las Vegas.
Thank you.
Author
Hi Dede, at the moment we don’t know of any recurrent UTI specialists in Las Vegas (this is sure to change in the future), but I sent you some information about clinicians who offer appointments via telemedicine. I hope it helps. Melissa
I cried reading this. I have suffered for so long. Is there someone in Southern California who can help? I would forever be grateful for any information. Thanks.
Author
Hi Beth, so sorry to hear you’re going through this. You’re not alone. I just emailed you some information and I hope it helps. Melissa
I’m living in Louisville, KY and have dealt with recurrent UTIs since January 2020. After two negative urine cultures, they’re now saying I have IC. But my symptoms feel just like when I had the recurrent UTIs. I’m seeing a Urologist who uses MicroGen testing but he almost never tells me the results, just puts me on antibiotics. I’m sensitive to several antibiotic families so I’m limited in what I can take. I’ve also met with a Urogynocologist (doesn’t do MicroGen) who confirmed I didn’t have any pelvic floor issues or an urethral diverticuli.
Is there anyone in the Louisville, Kentucky area you can recommend who specifically deals with rUTIs?
Author
Hi Tiffany, I just sent you an email with some more information. I hope it helps. Melissa
Hello, I was recently diagnosed with IC. For years I had chronic UTIs, but in the last year the tests all were coming back negative (positive for bacteria and leukocytes). Is there any doctors is Cleveland, Ohio that you recommend?
Author
Hi Alice, I just sent you an email with more information. Melissa
I’ve been waiting about an oral vaccine that is being used in Europe called Uromune. Are you familiar with this? I’ve read all the studies and they seem to make sense of that they would work
Author
Hi Patricia, we are aware of a number of different UTI vaccines available outside the US. We are currently working on some content on the topic and I hope to be able to publish that soon. Melissa
This would be wonderful. I saw that Uromune has some clinical trials running but I’m unclear about whether they’ll be available in the US. I’d jump on that in a heartbeat!
Author
Hi Salima, we’re monitoring the situation with UTI vaccines in the US and will be sure to publish something as soon as we have confirmation of any availability. Melissa
I have suffered from UTI’s and IC for over 40 years. The pain consumes my life. I’ve tried myrbetric and bladder installations. I’ve been told to try to relax my bladder, followed the bladder diet, bladder distention, supplements, the list goes on and on. Can you tell me if there is a doctor near Florence Alabama that is willing to try these methods.
Author
Hi Barbara, I just sent you an email with more information. Let me know if you have any questions. Melissa
Hi! Can you recommend anyone in Southern California? Been dealing with this for over a year now. Thank you!
Author
Hi Juliette, I just emailed you with more information. I hope it helps. Melissa
Hi there. This article was so helpful and has given me new hope…I wish my urologist took this approach. Could you recommend any practitioners in southeastern Michigan or anywhere in MI or Ohio that could help with my IC? Thanks so much for your time.
Author
Hi Christina, I just sent you an email with some information that I hope will be helpful. Melissa
Can I get additional information as well?
Author
Hi Sara, I’m not sure where you’re based, but I sent you an email with more information. Melissa
Hi Can you recommend anyone in the Mitchell, SD area?
Author
Hi Brenda, I just emailed you with some information on options you might consider. Melissa
Hello,
Do you have any recommendations for doctors following her protocol in the Atlanta-Georgia area or telemedicine? I’ve been suffering with recurrent UTI for years, recently I had kidney stones and a possible reactive arthritis in my right hand due to recent UTIs too. I’m 35 and showing signs of bone damage due to this reactive arthritis. Doctors just want to put me in immuno suppressants without investigating the root cause which I believe is properly treating the UTIs, I feel now my UTIs got even more my attention because of the joint prognosis. My insurance plan also covers out of state so if you know also any provider with similar protocols of Dr Kriz or Dr Michael Hsieh in other states too if there is no one in Atlanta. Thank you.
Author
Hi Caroline, I just replied to an earlier email you sent us, with more information. Melissa
I was diagnosed with IC in 2005. Have been on Elmiron until recently and got an Interstim in 2012. I stopped taking Elmiron because of reposts of side effects (vision loss) and having a lot of issues. Frequency and pain, but negative cultures.
I received my microgen results last week, positive for ureaplasma parvum and lactobacillus liners. Is there an embedded infection specialist in Michigan that may be able to help with treatment protocol?
My gyn ordered the test for me, but does not know how to treat.
Author
Hi Stacey, I just sent you an email with some options you might like to consider. Melissa
Hi there, I’ve been diagnosed with IC. I am wondering if you have any information about doctors that might help in New Mexico.
Author
Hi Megan, I just sent you an email with some possible options to consider. Melissa
I was just recently diagnosed with IC. Could you recommend a doctor in the Detroit area?
Author
Hi Vickie, I just sent you an email with some information on this. I hope it helps. Melissa
Can you recommend someone in the Portland OR area? I have been dealing with IC for 23 years.
Author
Hi Abby, I sent you an email with some information that I hope will help. Melissa