Recurrent UTI Testing Alternatives
Standard UTI testing methods are inaccurate and inadequate. This has been shown over and over again. There is evidence, there are studies, and there are females everywhere with recurrent UTI symptoms who keep getting negative UTI test results.
The inaccuracy of UTI testing is such a significant issue, we’ve written thousands of words explaining it in more detail. But it’s super interesting, trust us. Or don’t just trust us – read it to see for yourself!
Jump To Section:
- Better testing options for recurrent and chronic UTI. >>>>
- Standard urine culture testing tips (if this is your only option). >>>>
- Why it’s essential to find the right practitioner. >>>>
- How to talk to your doctor about recurrent UTIs. >>>>
There’s no denying that urinary tract infections are largely a female health issue. One that has been overlooked for far too long.
Support groups and political campaigns across the world are gaining momentum in their fight for better UTI testing, diagnosis and treatment. Success will mean better testing and new guidelines for recurrent urinary tract infections, chronic cystitis and other chronic urinary tract conditions.
In the meantime, a number of researchers, specialists and doctors in various countries have developed more comprehensive approaches to conditions such as recurrent UTIs, chronic cystitis and Interstitial Cystitis.
Thanks to their efforts, there are a few alternative testing options you may wish to consider. Some specialists use microscopy of a fresh urine sample, Expanded Quantitative Urine Culture (EQUC) or Next Generation Sequencing (NGS) and have found these to be significantly more accurate than the standard urine culture test.
So much so, that they have been able to identify and treat a bacterial cause for persistent UTIs and in many cases, Interstitial Cystitis, when standard testing failed to provide useful results.
 | “For the cases I see, on average it takes a year of antibiotic treatment to resolve their symptoms, but there’s a wide variance." |
Gaining access to these alternative testing methods could mean a commitment of time and money on your part, but it may provide you with an answer where standard UTI testing has failed to.
Like others before you, you may find a solution, and finally overcome your chronic symptoms once and for all. Read on for further details.
Better UTI Testing Options For Recurrent UTIs
More accurate UTI testing methods like microscopy, Expanded Quantitative Urine Culture (EQUC) and Next Generation Sequencing are not yet widely available, but you may be able to access them, so we’ve outlined some useful information below.
Next Generation Sequencing UTI Testing
Although scientists have used DNA to identify microbes for many years, the technology has been expensive and time consuming, and therefore considered inappropriate for everyday testing of chronic illnesses.
This is changing, however, and the latest technology is now being used to identify the unique DNA of microbes found in human test samples, including urine. DNA testing has already detected more than 1,200 different microbial species in urine samples – a number far higher than any other UTI testing method.
Some chronic UTI literate practitioners are wary of NGS testing, as it has the ability to detect hundreds of organisms in a single urine sample, and the significance of these organisms is not yet known.
We now know that urine is not sterile, but research into the urinary microbiome is still fairly recent, and we do not yet have a solid understanding of it. If NGS testing detects hundreds of organisms, how do we know which to treat?
To help address this question, NGS results typically show what percent each organism was found in – the idea being that any dominant pathogens will be identified, and that these should be looked at first when it comes to treatment.
This approach has proven very successful for many practitioners embracing NGS testing in different areas of human health, including chronic urinary tract issues.
NGS testing has been able to identify the cause of chronic illness where conventional testing has not, enabling many sufferers of long term illness to recover and return to their pre-illness lives. This includes a multitude of chronic UTI and Interstitial Cystitis sufferers.
If conventional UTI testing methods have failed to provide you with answers, NGS testing could finally help you find them.
Because NGS testing does not involve growing microbes, samples are not easily affected by time, temperature or antibiotic use, and all bacteria and fungi can be tested within a single test, from one urine sample.
There are a few different types of NGS testing, with varying levels of accuracy.
Aperiomics: Deep Next Generation Sequencing Test For UTIs
Aperiomics uses deep metagenomic sequencing, an unbiased genetic sequencing technology that allows them to create a complete genetic fingerprint of all microorganisms in any sample you provide.
In short, this technology looks for every known microorganism in a single test.
Aperiomics is based in Virginia, USA, and is currently the only provider of this type of testing, globally. Their database of microbes contains more than 37,000 microorganisms, making it the most comprehensive in the world. If there is a specific pathogen or pathogens causing your UTIs, they are confident they will identify the issue.
 | “The traditional health-care system has never had the right tools to see what’s going on. We have the tool, and our goal is to change everything about how infections are identified.” |
You can order a kit directly from the Aperiomics website, and ship your sample from within the USA, or internationally.
We’ve covered the testing offered by Aperiomics in great detail here. So you can learn more about whether it’s right for you.
Or, if you’re ready to order a test, you can find the right order page by clicking here for patients, and here for practitioners.
MicroGenDX: Next Generation Sequencing Test For UTIs
MicroGenDX, a US based molecular laboratory, uses NGS testing and states that their tests identify 100% of the known microbes in a urine sample from a database of >30,000 species, with 99.9% accuracy.
Simply speaking, they extract the DNA of bacteria, fungi and parasites from your urine sample, then match these to their database, and report on what they find, using two different technologies.
In addition to breaking down the percentages of all microbial species detected, antibiotic resistance genes for 8 antibiotic classes are also predicted by MicroGen DX, and their report will contain recommendations about which antibiotics they believe will be most effective.
 | “We strongly believe MicroGenDX Laboratory can provide better diagnostic information to treat chronic UTIs by utilizing Next-Gen Sequencing. NGS takes the guesswork out of microbial detection allowing for targeted utilization of antimicrobials." |
You can order a kit directly from the MicroGenDX website, and ship your sample from within the USA, or internationally.
We’ve covered the testing offered by MicroGenDX in great detail here. So you can learn more about whether it’s right for you.
Or, if you’re ready to order a test, you can find the right order page by clicking here for patients, and here for practitioners.
And as we mentioned above, it helps to have your test results interpreted by a practitioner who has experience treating chronic urinary tract conditions.
 | Long term urinary tract issues may be caused by a chronic bladder infection which will require a treatment regimen that is considerably different to that of a single UTI. There are very few practitioners trained in this type of treatment, so it pays to do a little research and find one with experience. |
If you’re interested in NGS UTI testing, you can talk to your own doctor about ordering a test, or take a look at our guide on recurrent UTI treatment, for more information on practitioners that can help.
Urine Broth Culture Test
The standard urine culture test uses agar to encourage the growth of pathogens over a 24-48 hour period. Urine broth culturing uses a Trypticase Soy Broth (TSB) over a period of 3-6 days.
Broth is a liquid, whereas agar is put on a dry culture plate. If you consider it, it makes total sense for bacteria that like to grow in a liquid such as urine, to grow more easily in a liquid broth, than on a dry plate.
And logically, it’s not so surprising that researchers have managed to identify multiple types of UTI-causing bacteria more accurately using broth culture UTI testing techniques, than with standard urine culturing.
The urine broth culturing method also includes procedures to test for and remove antibiotics and body waste products from the urine before incubation.
Effectively, your urine sample is ‘cleaned’ before it is incubated.
Culturing a urine sample using the broth method is reported to allow more microbial strains to emerge from the urine sample, and therefore provide more accurate results than a standard urine culture.
Specific pathogens are isolated from the broth-incubated sample, and antibiotic or anti-yeast sensitivity testing is conducted in order to identify the most appropriate treatment.
The broth culture technique was pioneered by the late Dr. Fugazzotto, who achieved notable success using this method.
This type of broth culture, however, has not yet been backed by extensive research and United Medical Lab, the only laboratory that did offer the test, ceased doing so as of May 2019.
Fresh Sample Urine Microscopy Test
This test is exactly what it sounds like. Upon providing a urine sample, it is immediately analyzed under a microscope to count things such as bacteria, fungi, white and red blood cells, and bladder lining cells (epithelial cells). It’s a technique that was used in the 1920s and has since been revived.
One UK specialist, Professor Malone-Lee, is particularly known in the field of chronic urinary tract infections and Interstitial Cystitis and uses this UTI testing technique in combination with a thorough assessment of symptoms. Professor Malone-Lee has successfully treated thousands of patients with urinary tract conditions previously considered untreatable.
 | "We do one test; immediate microscopy of a fresh specimen of urine; counting the white and red blood cells, bladder lining cells, bacteria and fungi. The symptoms and the microscopic data are interpreted...they force consideration of all the data particularly the patient's narrative." |
At present, we are unaware of US-based specialists using this same set of testing and assessment techniques, but will provide updated information as it becomes available.
Standard Urine Culture Testing Tips
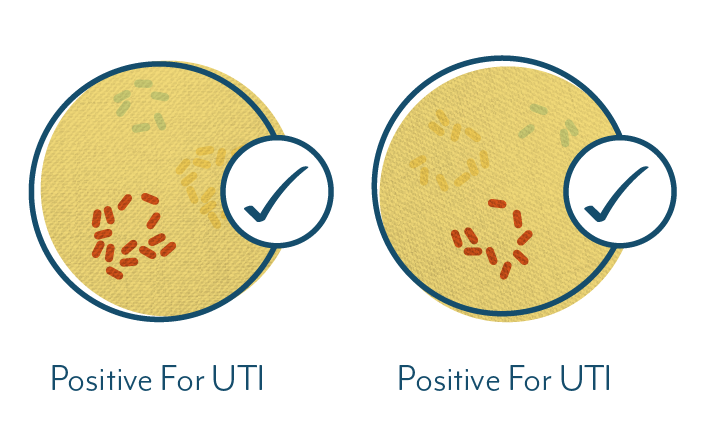
Although we know standard UTI testing is inaccurate, some individuals do find an answer.
 | “I got this UTI that just would not go away. After a few rounds of antibiotics my doctor had my urine tested. The results showed the cause of my UTI was a different bacteria than she first suspected. She gave me a different antibiotic and it worked!” |
Standard UTI testing may be a road you wish to go down, particularly if you have not had your urine tested and you get acute UTI symptoms regularly.
Given the issues with UTI testing (which we’ve described in our UTI Test section), we thought we’d provide a few tips below on increasing the likelihood of getting an accurate result with standard urine testing, should you choose to pursue it.
While we don’t usually recommend using techniques that have been shown to be so flawed, there are very few options for UTI testing in most regions. So instead of dismissing it completely, let’s discuss how you can get the most out of what’s available.
As we covered in our testing section, one of the issues with the standard urine culture test is that the threshold for bacteria concentration in the urine is too high to catch many infections.
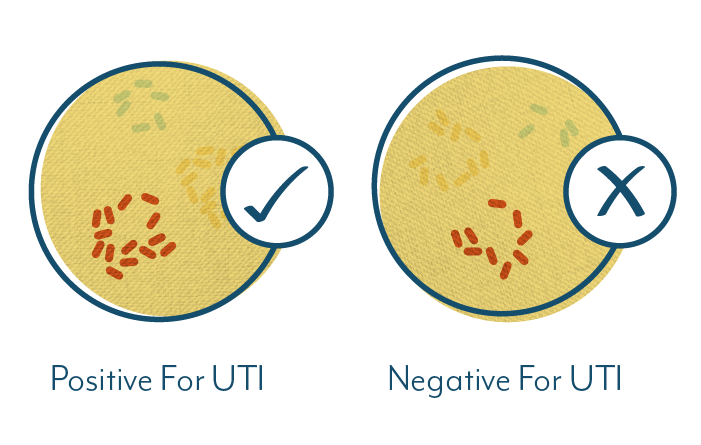
While many labs still use the threshold of a minimum colony forming unit (CFU) count of 105 per milliliter of cultured urine, females with symptomatic UTIs may present with CFU counts as low as 102/mL. For this reason, a number of recent guidelines recommend decreasing the threshold to 103/mL.
In plain language, a cut off point of 105 CFU/mL means your cultured urine sample could contain 90,000 colony forming units of bacteria per milliliter, but because the threshold is set at 100,000 (105), your test result will be reported as negative.
This doesn’t necessarily mean you should accept that answer.
 | “There’s an old expression, if it looks like a duck, walks like a duck, and quacks like a duck. It's gotta be a duck. And so to have somebody who has pain, urgency, frequency and burning, and yet they're told they don't have an infection because a urine culture was negative, who do you believe? Are you treating a lab result? Or are you treating a person?” |
Getting back to standard urine testing… On top of the issues with the CFU threshold, some guidelines suggest the standard incubation time of 24-48 hours may be insufficient to grow all pathogens present in a urine sample.
Certain types of bacteria or fungi may be much slower growing, and will only appear in significant concentrations after 3-5 days. It is also believed that some pathogens may never grow on an agar plate, which is the standard technique used for UTI testing.
What does this mean for you?
 | If you are unable to access more accurate UTI testing methods, and choose to have your urine cultured via the standard UTI testing method, you can request: |
If you are unable to access more accurate UTI testing methods, and choose to have your urine cultured via the standard UTI testing method, you can request:
- The colony forming units (CFU) threshold be decreased from 105 to 103.
- A susceptibility test be completed if your test is positive for bacteria or yeast. This should be done automatically, and is essential to identify which antibiotic or anti-yeast treatment should be prescribed.
- A longer incubation period, to encourage the growth of more types of pathogens.
These changes aren’t always possible, so you should ask your doctor about it, or request it directly at a lab if you test independently.
In the US, you have the right to pursue UTI testing independently, and the right to request your lab test results without seeing a doctor first. This is not the case in all countries.
If your test is negative, you can discuss this with your doctor or lab. It may make sense to conduct another test at a different time of day (see our tips below), or to test for different pathogens that could be causing your symptoms.
Given the inaccuracies of standard UTI testing, a negative result may also be a prompt to pursue more accurate testing methods, like those above.
How To Collect A UTI Testing Sample Like A Pro
Whether you opt for standard urine culturing, urine broth culturing or Next Generation Sequencing, you’ll need a top notch urine sample for the most accurate results. Fortunately, all three testing methods require urine to be collected in the same way.
 | "I’ve provided so many urine samples now, but I’m never sure how full the container should be. So I make it different each time, hoping the doctor will say ‘oh wow, that’s way more than we need,’ or maybe, ‘great job, that’s perfect.’ But he never reacts. His poker face is unbreakable." |
There’s no need to worry what your sample looks or smells like. After all, that’s why you’re getting tested – because there is an issue. We’re sure you’re doing a good job already, but here are a few tips to check your urine sample technique against:
 1. Wash your hands. Then use disposable gloves if possible. |
|
| 2. Remove the sample container lid, being careful not to touch the inside. Place the lid face down on a clean tissue. | |
| 3. If you’ve been supplied with cleansing sponges, use them to clean the area around your urethra - this helps minimize contamination from other organisms. Avoid touching your urethra or the area around it with your hands. | |
| 4. Find a position over the toilet that seems viable for getting urine in the container and NOT on the floor. Some people prefer to straddle the toilet backwards. | |
| 5. Use your fingers to hold the folds of skin around the vagina away from your urethra, and keep holding until you have collected your sample. This also helps minimize contamination. | |
 6. Urinate first into the toilet for a second or two, then without stopping, aim for the sample container, filling it to about two-thirds (there’s your answer to the, ‘Is this enough? Is this too much?’ question). |
|
| 7. Congratulate yourself on getting it mostly into the container. | |
| 8. Continue urinating into the toilet until your bladder is empty. | |
 9. Without touching inside the container or lid, screw the lid back onto the container. |
|
| 10. Use paper towel to wipe off excess urine on the outside of the container (this isn’t a rule, but we know you missed at least a little bit). | |
| 11. Wash your hands! |
If you’re posting your sample, you will most likely be given a few additional instructions on how to make your sample fit for shipment. Pay close attention to these!
 | For A UTI Test At Home, Always Keep A Urine Test Kit Or Sample Container On Hand. Why? |
If standard UTI testing is your only accessible testing option, you’re more likely to get an accurate result if you collect your urine sample at the height of your symptoms. Symptoms tend to flare up when the concentration of bacteria in your bladder increases, so this is the perfect time to get a snapshot of what is happening in your urine at that moment.
If you suffer from recurrent UTIs, ask your doctor or your chosen lab for a sterile sample container to take home or order one online. Make sure this is provided inside a sterile package, to prevent contamination before you need to use it.
Next time you get acute symptoms, pee in that container before you start guzzling fluids, trying home remedies, or popping pills. Drinking excessive amounts of fluids before collecting your sample will only dilute your urine, decreasing the likelihood of an accurate test.
Other things to avoid before collecting your sample:
- Diuretics
- Antibiotics
- Vitamin C
And while you obviously can’t control the timing of a UTI, it helps to collect a urine sample when you are not menstruating. Menstrual blood can contaminate your sample and affect your test results.
Taking a sample at the height of your symptoms, and before intervention, gives you the highest chance of an accurate test.
Put your urine sample in a sealed plastic bag, and drop it in to your doctor or lab within an hour. If you can’t manage that, you can store it in the fridge for up to 24 hours.
If you’re shipping it via overnight express post, pack it with dry ice or an ice pack to keep it cold.
Oh, and put your name on your sample container BEFORE getting to the doctor or lab. Or be prepared to put it on display and name it while you’re there.
If you don’t have a sterile sample container on hand, do your best to get to the doctor or lab asap.
If you’re in the habit of popping antibiotics at the first sign of a UTI, think twice, and get tested first.
 | For chronic or ongoing low level UTI symptoms without acute episodes, the best time to collect a urine sample is first thing in the morning. Your urine is at its most concentrated after hours of sleeping and not peeing. A higher concentration of any potential pathogens may provide a better chance for an accurate result. |
 | “When my first round of UTI testing came back negative my doctor had me submit urine samples at 3 different times throughout the day, over the course of a week. She found a huge amount of bacteria in my morning urine samples. I got the right antibiotic, and miraculously, after 15 years of recurrent UTIs, I was suddenly free of symptoms!” |
If you have previously had your urine tested, only to receive inconclusive or negative results, it could be worth submitting multiple urine samples, at different times of the day, to track the presence of pathogens in your urine.
Ultimately, you may never get an accurate test result from standard UTI testing, and it’s always better if you can pursue a more accurate alternative.
Why It’s Important To Find The Right Practitioner
While you may be able to request UTI testing independently, the results have limited usefulness without a practitioner who can interpret the information and prescribe an appropriate treatment regimen.
In the case of recurrent or chronic UTI, this isn’t as simple as taking the results to your local doctor. Persistent urinary tract infections may be caused by a chronic, embedded infection in the bladder called a biofilm. We’ve covered this in more detail in our guide on Chronic Urinary Tract Infection vs. Recurrent UTI.
What you need to know here, is that a persistent, chronic infection is unlikely to respond to a standard short course of antibiotics that would typically be prescribed for a UTI. Instead, it can take several months of continuous, specialized treatment for symptoms to dissipate and for the bladder to heal.
You may have had a chronic urinary tract infection for years, and it can take just as long to heal it.
Long term treatment must be monitored by an experienced practitioner. You can find out more about the options in our UTI treatment guides.
How To Talk To Your Doctor About Recurrent UTI
 | Get Your UTI Test Results Organised! |
- Request copies of your previous UTI testing results. You can do this yourself by calling clinics that have arranged testing for you, or you can ask your doctor to make these requests on your behalf.
- Always ensure you receive a copy of any future test results and store all your results in chronological order for easy reference.
- Familiarize yourself with your historical results. Note any patterns and anything that stands out. Highlight specific aspects that seem unusual and make note of any questions you have regarding your results.
- When you are ready, take your collated results and questions to your doctor. This information can be very valuable, particularly when you find the right practitioner – who is willing to investigate your recurrent UTIs further.
- Arm yourself with knowledge and references regarding recurrent/chronic UTI – you should be prepared to discuss this concept, and to stand your ground.
- If your doctor is unwilling to listen to your concerns, you should feel empowered to search for a practitioner who will.
 | “I’d had so many UTIs and so many lab tests at different clinics. I always made sure I got a copy of my results. Every test showed low levels of something, but no full blown infection. Showing my results to my own doctor helped her piece together the fact that I did have a chronic infection. That was a turning point for me.” |
Share your questions and comments below, or get in touch with our team.

I had a kidney stone in January of this year. Since then I have had recurrent UTI’s. Usually every time after sex. My urologist says its not related to the kidney stone. My Gyno gave me a scrip for Macrobid 100mg, to take before or after sex, but I am a little apprehensive because of possible side effects. I am able to most times flush the infections with D-mannose, cranberry pills and lots of water, but I don’t think I’m really getting rid of it completely. I only take the regular antibiotics if it gets really bad. Any thoughts?
Author
Hi Lee anne, you may have already read our info on chronic infection and how it can remain an issue without sufficient treatment. We’ve listed some treatment approaches by chronic UTI specialists here, which may help. If you have other specific questions or would like further info about chronic UTI practitioners, you can email me. Melissa
I’m sure you’ve already read about this since you made it all the way to this website, but do you pee every time you’ve had sex? Like shortly afterwards?
Author
Hi Jenny, you’re right – I think most people with recurrent or chronic UTI have already been doing ‘everything right’, including peeing after sex. You can have ‘perfect hygiene’ and still experience recurrent UTIs! While it’s always good to consider prevention, often a more proactive approach is needed. Melissa
My mother is 85 years old and is generally in very good health but she has had problems with recurrent UTI’s over the past few years. In the past 12 months, she has had about 6 confirmed UTIs, although there have been other occasions where she is sure she has an infection but the tests come back negative. When she has a UTI, she suffers from dizziness and severe shortness of breath. None of her doctors seem to believe that these symptoms are related to a UTI, but we believe they are. She has had her heart and pulmonary system checked multiple times and they have found no defects. We would like to pursue NGS testing, but it appears both labs require that the tests be ordered by a medical practitioner? Can you offer any advice please?
Author
Hi Susan, sorry to hear your mother is experiencing that. The testing requirements tend to differ per state in the US, so depending where you are, you may be able to order a test without going through a doctor first. Having said that, it’s essential to find a practitioner who is able to interpret the results, and discuss the best treatment approach with you. Most practitioners are unfamiliar with this type of testing. I can provide some further info if you get in touch directly, or you could reach out to the two companies we’ve listed above to discuss options. Melissa
Hi Melissa,
Thank you for your feedback. My mom has an appointment with a urologist on 9/4, so I’ve printed out information from the website and links to the two labs for her to take with her…..I’m hopeful he will be open to the idea of NGS testing, but if not I’ll try contacting the labs directly to see if they have any suggestions.
Author
Hi Susan, good luck. I got your direct message too, so I’ll respond to that asap. Melissa
After going over 30 without a single UTI (I used to get them regularly) I am now suffering with constant bouts, even though 1 culture and I quick test both came back negative. I was prescribed Nitrofurantn 100 mg and it relieved my symptoms but they quickly came back after I was finished with prescription. I then went to another doctor because I couldn’t get into see my original doctor and he gave me 20 doses of Cefuroxime 500 mg. All my symptoms are back and I’m going crazy. But sometimes during the day, the symptoms subside, a little. I live near Seattle. Can anyone recommend a good urologist?
Author
Hi Sherrie, your story is similar to many we hear every day. A very frustrating situation to be! I sent you some info in response to your email. I hope you find answers soon! Melissa
I went to the doctors tested positive for chlamydia this was two years ago I’ve done anywhere from 100 to 200 samples all came up negative but I’m still having an urgency to Pee in a burning sensation all the time that won’t go away what can I do next
Author
Hi Grant, you may like to discuss with your doctor the alternative testing methods described above. Some treatment approaches are covered here. If you’d like more info on finding a practitioner, you can send me a direct message. Melissa
My mother 69 years is having uti within 10 days treatment with niftran for 3 episodes . Routine urine shows microorganins present but culture shows no growth.
Author
Hi, if you haven’t already, you may like to read about chronic UTI specialists and different approaches that could help. You can also reach out to us if you’d like more specific information. Melissa
I have had recurrent UTIs over the last 6 months. A more extensive lab test identified the source as a staph infection. Does this change how the UTI is treated?
Author
Hi Linda, only your practitioner can properly answer that. I’m interested in hearing more if you’d like to discuss it though! Melissa
Can I still have infection even if lab results say ‘no growth?’
Author
Hi Laura, standard urine cultures have been proven unreliable, so it is entirely possible an infection exists, even if it is not picked up by this type of test. You can read more about why urine culturing is unreliable on our site. I’ve also replied to your email with more info! Melissa
I have interstitial cystitis and was wondering if this test could help me and if so what Dr. in my area would do them. I live in Ohio. Thanks
Author
Hi Ashley, there are a few practitioners in the USA who are using these types of testing for IC patients, and they have reported success in identifying the potential cause of the issue in many patients. Any practitioner in the USA can order these tests, however, it helps to work with one that has experience in interpreting the results, and recommending an appropriate treatment plan. You might like to get in touch with one of the practitioners listed on our site for more information on how best to go about this.